Introduction
- Cardiac tamponade is a life-threatening condition that requires prompt recognition and management.
- It is a clinical diagnosis supported by echocardiographic findings.
- Definitive treatment involves pericardiocentesis or surgical intervention.
Pathophysiology
- The pericardium consists of two layers surrounding the heart.
- Normally minimal fluid within this space, usually less than 50ml.
- Accumulation of fluid results in high intrapericardial pressure leading to compression of the cardiac chambers.
- Typically right chambers (low pressure systems) are more likely to be compressed than left chambers (high pressure system).
- Unchecked rising intrapericardial pressures will lead to collapse of cardiac chambers eventually leading to hypotension, shock, circulatory collapse and typically PEA (pulseless electrical activity) cardiac arrest.
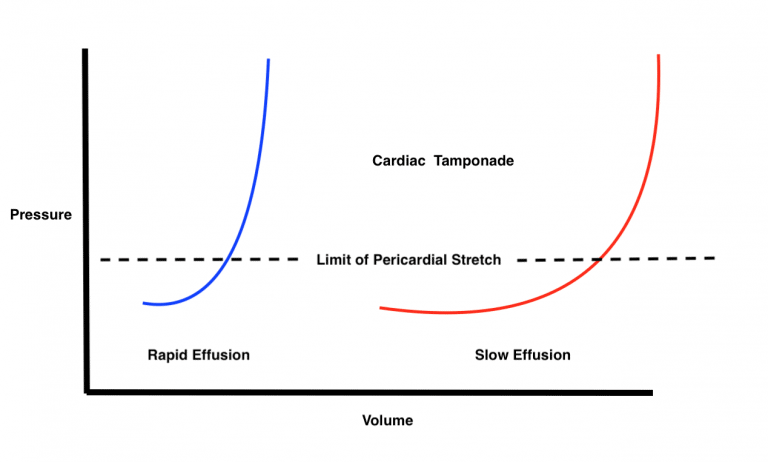
- No specific amount of fluid will necessarily cause cardiac tamponade. Small amounts (e.g., 200ml ) that occur acutely can cause tamponade; meanwhile, a patient with a litre of fluid in the pericardial space may not be in cardiac tamponade. Slowly accumulating pericardial effusions will give the pericardium time to stretch and accommodate to changes in pericardial pressure.
Ventricular Interdependence
- Ventricular interdependence is the concept that changes in one ventricle affect the other ventricle.
- This phenomenon is seen in cardiac tamponade as well as other conditions such as constrictive pericarditis.
- In normal physiology during inspiration, negative intrathoracic pressure is transmitted to the cardiac chambers, lowering the external pressure on the right ventricle and causing increased venous return to the right heart. The right heart can normally accommodate this increase in venous return.
- Increased right side filling pressures > reduced left ventricular pressures. In cardiac tamponade, the right ventricular free wall is constricted by the pericardial effusion. This results in “bowing” of the intraventricular septum into the left ventricle causing a reduction in left ventricular filling.
- This concept is seen clinically in the form of “pulsus paradoxus.”
Diagnosis
Physical Exam
- Tachycardia, tachypnea, hypotension, hypoperfusion
- “Pulsus paradoxus”: reduction of systolic blood pressure >10mmHg on inspiration.
- Calculated using sphygmomanometry.
- The difference between the onset of Korotkoff sounds in expiration only vs when they are audible throughout respiratory cycle is the pulsus paradoxus.
- In the critical care setting, this can be seen on arterial BP monitoring.
- Cardiac findings
- Muffled heart sounds
- Elevated JVP
- Blunted Y-Descent on JVP
- Classic Beck’s Triad (hypotension, muffled heart sounds, elevated JVP) although all 3 are rarely present together.
Clinical Pearls:
Differential for pulsus paradoxus: Constriction, pulmonary embolism, right-ventricular infarction, severe pulmonary diseases (asthma/COPD), severe hypotension.
Differential for tamponade in the absence of pulsus paradoxus: right/left ventricular hypertrophy, severe left-ventricular dysfunction, severe hypotension, localized effusion, pericardial adhesions, aortic regurgitation, atrial-septal defect.
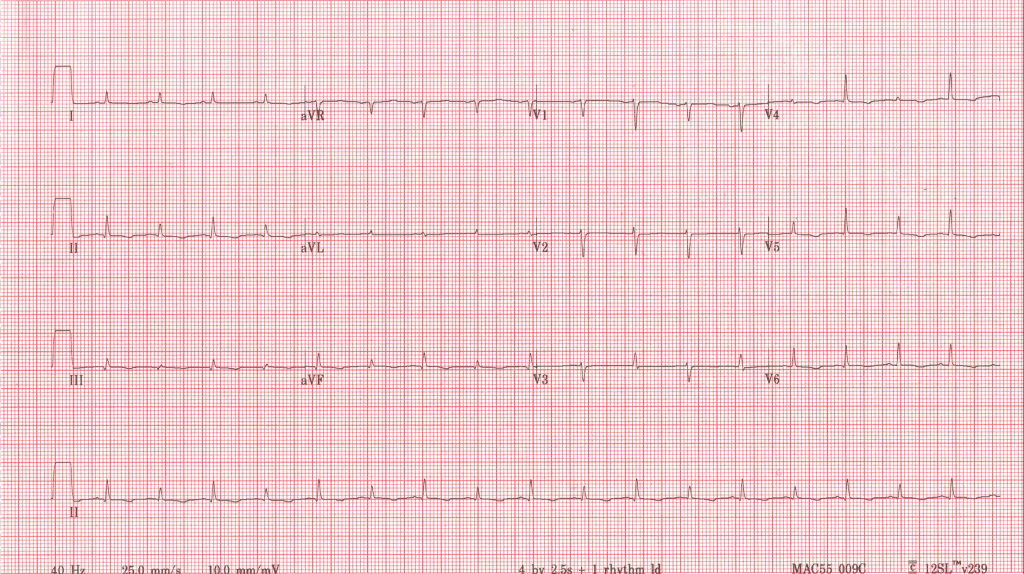
ECG
- Low Voltage
- Electrical Alternans (alterations in QRS amplitude beat-to-beat)
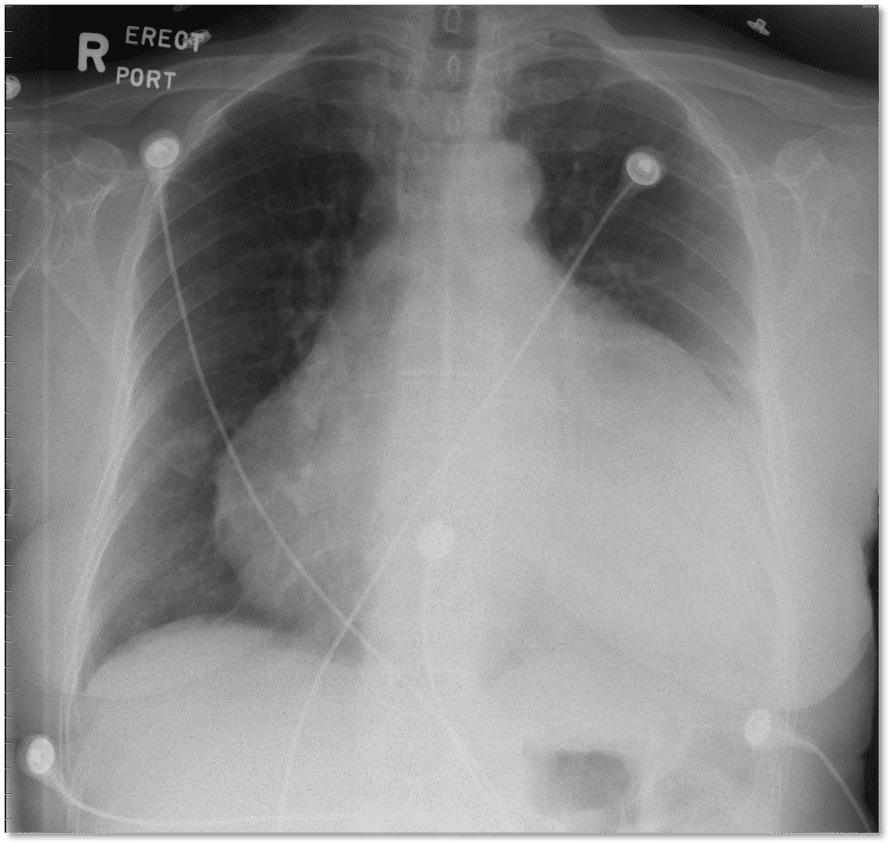
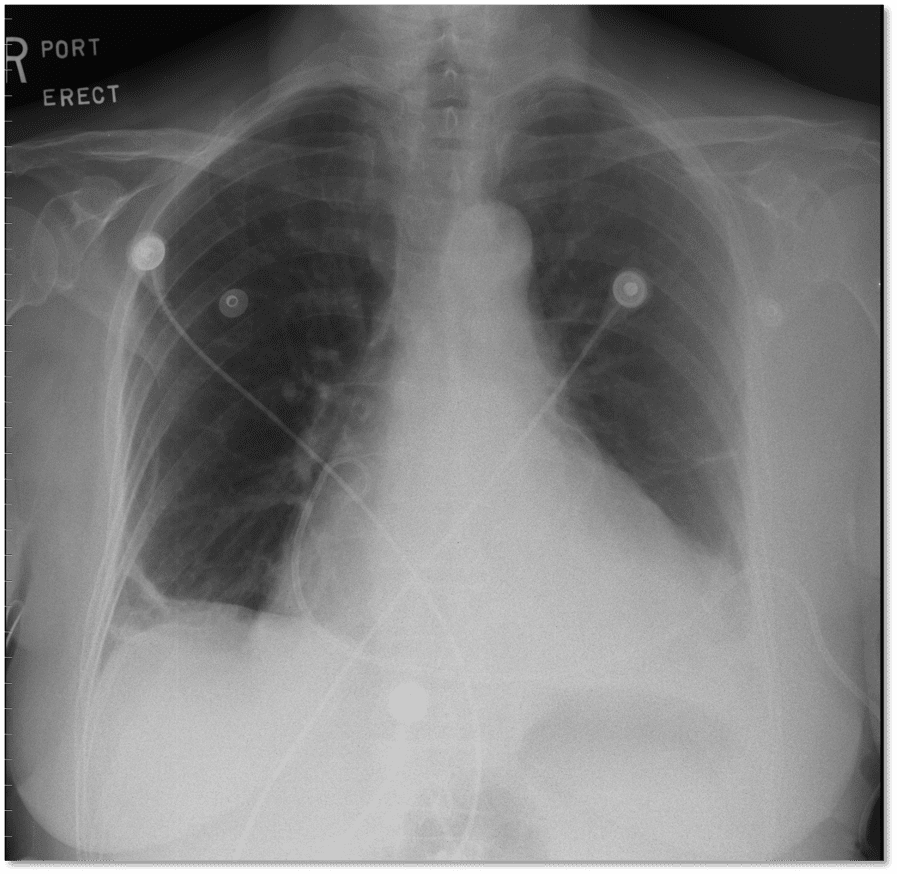
CXR
- Enlarged cardiac silhouette can be seen in slowly developing effusions
- Important to assess for other causes of symptoms/shock (Exp Tension Pneumothorax)
- CXR is not sensitive or specific for cardiac tamponade.
Fluoroscopy
- Abolition of cardiac pulsations.
Echocardiogram
- Echocardiogram/POCUS is an important test to assessing for pericardial effusion and determining the size, location, and hemodynamic consequences of the effusion. Remember that cardiac tamponade is a clinical diagnosis. Echo is supportive of diagnosis.
- Chamber Collapse
- This is commonly seen in cardiac tamponade.
- It occurs when intrapericardial pressure exceeds pressures in the cardiac chambers.
- Typically, the right-sided chambers will be affected first since they are lower pressure systems.
- Right atrial diastolic collapse of greater than 1/3 of the cardiac cycle is specific/sensitive.
- Right ventricular diastolic collapse is very specific, though it may not occur in cases of right ventricular hypertrophy.
- Left atrial collapse is uncommonly seen since left-sided pressures are higher, but is more specific for cardiac tamponade.
Circumferential pericardial effusion with probable RV diastolic collapse.
Short axis confirms RVOT collapse in diastole suggestive of tamponade physiology.
Apical 4 chamber showing RA diastolic collapse.
- Plethoric IVC
- Highly sensitive but not specific for cardiac tamponade as many conditions can cause dilation of the IVC.
- If the IVC is small and collapsing should re-visit the cause of the patients shock state since typically cardiac tamponade will have high right-sided pressures.
Dilated IVC with no respiratory variation suggestive of high-right sided filling pressures.
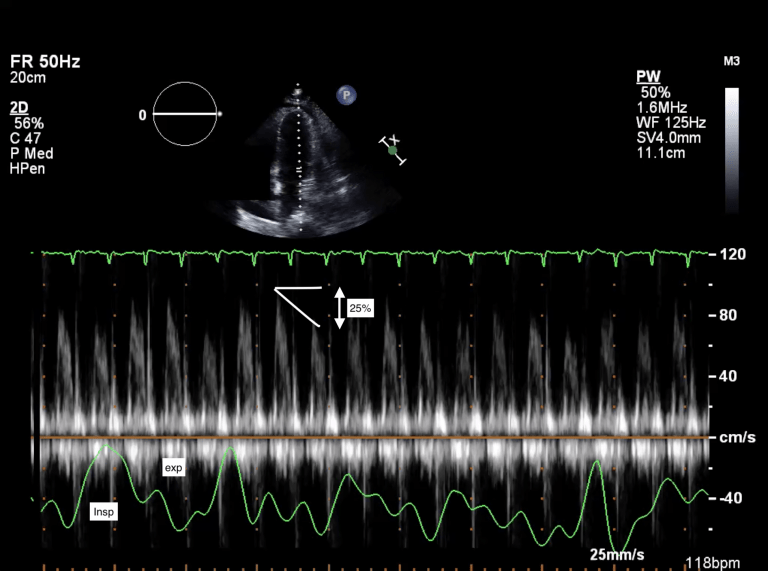
- Respiratory variations with flow
- Using pulse waved Doppler, mitral and tricuspid inflow velocities can be assessed for tamponade. This is the echo assessment of ventricular interdependence and pulsus paradoxus.
- Typically, a variation of 25% or more in the mitral inflow and 40-60% in tricuspid inflow with respiration is significant.
- In addition, visually abnormal septal bowing into the left ventricle may be seen with respiration.
Clinical Pearl:
In post-cardiac surgery patients may not have circumferential pericardial effusions and in fact can have very focal hematomas that cause “regional tamponade”. Other typical physical, hemodynamic, or echo features may be absent including pulsus paradoxus.
Echo dense material surrounding the RV suggestive of hematoma.
Large hematoma post-cardiac surgery externally compressing the RA causing tamponade.
Right Heart Catheterization (Swan-Ganz)
- Although not typically needed for diagnosis, right heart catheterization (RHC) may be helpful or add additional information support when the diagnosis is uncertain.
- The classic finding in RHC is the equalization of diastolic pressures between cardiac chambers.
- In addition, ventricular interdependence may be seen as an increase in right sided pressures results in a decrease in left-sided pressures. Remember the physiology!
Management
- Definitive management if pericardiocentesis or surgical intervention/pericardial window.
- Post-cardiac surgery related tamponade requires immediate consultation with cardiac surgery and typically surgical exploration.
- Fluids may be helpful to temporize hemodynamics by increasing preload.
- Pressors can be added to hypotensive patients to stabilize while awaiting definitive management.
- Please see our module on pericardiocentesis: http://www.cardioguide.ca/pericardiocentesis/
Authors
- Authors: Dr. Daniel Durocher (MD, FRCPC, Cardiologist, ICU Fellow)
- Graphics from Dr. Daniel Durocher and Dr. Craig Ainsworth (Cardiologist and Critical Care)
- Staff Reviewer: Pending (MD, FRCPC[Cardiology])
- Copy Editor: Megha Shetty, MD Candidate