Introduction
- Syncope is defined as loss of consciousness due to cerebral hypoperfusion, characterized by a rapid onset, short duration, and spontaneous complete recovery.
- A good history and physical examination are critical in identifying causes of syncope.
- Approximately 40% of people faint at least once in their life.
- Evaluation of the patient should answer:
- Is there a serious underlying cause that can be identified?
- What is the risk of a serious outcome?
- Should the patient be admitted to hospital evaluation?
Definitions and Differential Diagnosis
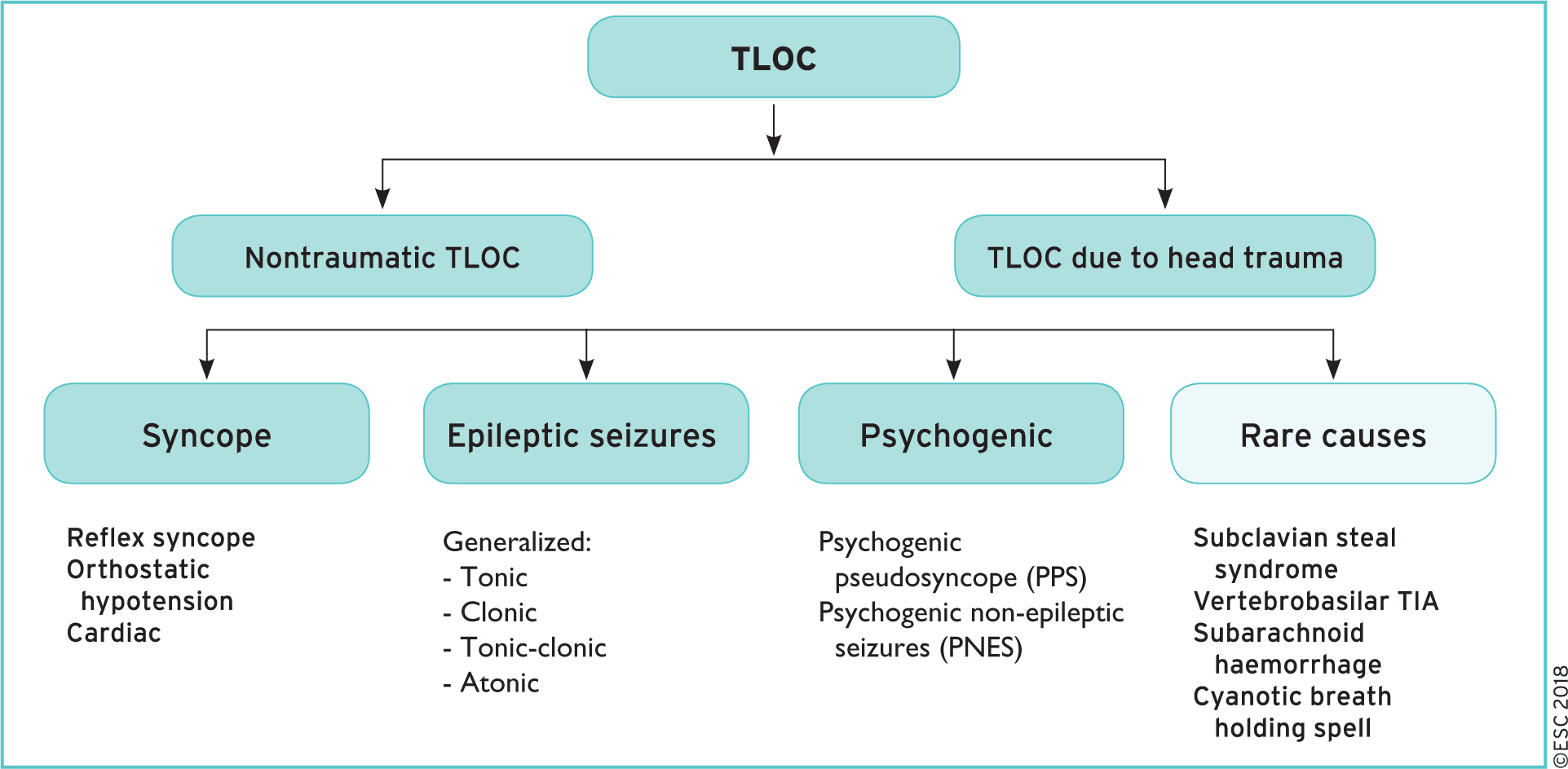
- Transient Loss of Conciousness (TLOC) is a broad category split into nontraumatic and traumatic causes
- Syncope is defined as a TLOC due to cerebral hypoperfusion, characterized by rapid onset, short duration, and spontaneous complete recovery
- Presyncope is defined as the signs and symptoms (prodrome) before syncope, with or without a subsequent LOC
- Seizures, pseduo-coma, intracranial hemmorrhage, TIA, metabolic disorders, intoxication and cataplexy can be falsely diagnosed as syncope. Click here for full list.
Pathophysiology and Classification of Syncope (ESC)
- Causes of syncope all lead to the same result: fall in systemic BP and resulting cerebral hypoperfusion (defining feature of syncope)
- Mean Arterial Pressure = Cardiac Output x Systemic Vascular Resistance. Thus each of the following causes a decrease in cardiac output and/or peripheral resistance.
1. Reflex (neurally mediated) syncope
- Vasovagal:
- Orthostatic VVS: standing, less common sitting
- Emotional: fear, pain (somatic or visceral), instrumentation, blood phobia
- Situational:
- Micturition
- Gastrointestinal stimulation (swallow, defaecation)
- Cough, sneeze – post-exercise
- Others (e.g. laughing, brass instrument playing)
- Carotid sinus syndrome
- Non-classical forms (without prodromes and/or without apparent triggers and/or atypical presentation)
2. Orthostatic Hypotension
- Drug Induced: vasodilators, diuretic
- Volume depletion: dehydration, hemorrhage, vomiting, etc.
- Primary autonomic failure: Parkinson’s disease, multiple system atrophy, Lewy body dementia
- Secondary autonomic failure: Diabetes, amyloidosis, spinal cord injuries, renal failure
3. Cardiac:
- Bradycardia: sinus node dysfunction (including bradycardia/tachycardia syndrome) – atrioventricular conduction system disease (ie. complete heart block).
- Tachycardia:
- Supraventricular
- Ventricular
- Structural cardiac: aortic stenosis, acute myocardial infarction/ischaemia, hypertrophic cardiomyopathy, cardiac masses (atrial myxoma, tumours, etc.), pericardial disease/tamponade, congenital anomalies of coronary arteries, prosthetic valve dysfunction
- Cardiopulmonary and great vessels: pulmonary embolus, acute aortic dissection, pulmonary hypertension
Note: LOC has four specific characteristics: short duration, abnormal motor control, loss of responsiveness, and amnesia for the period of LOC
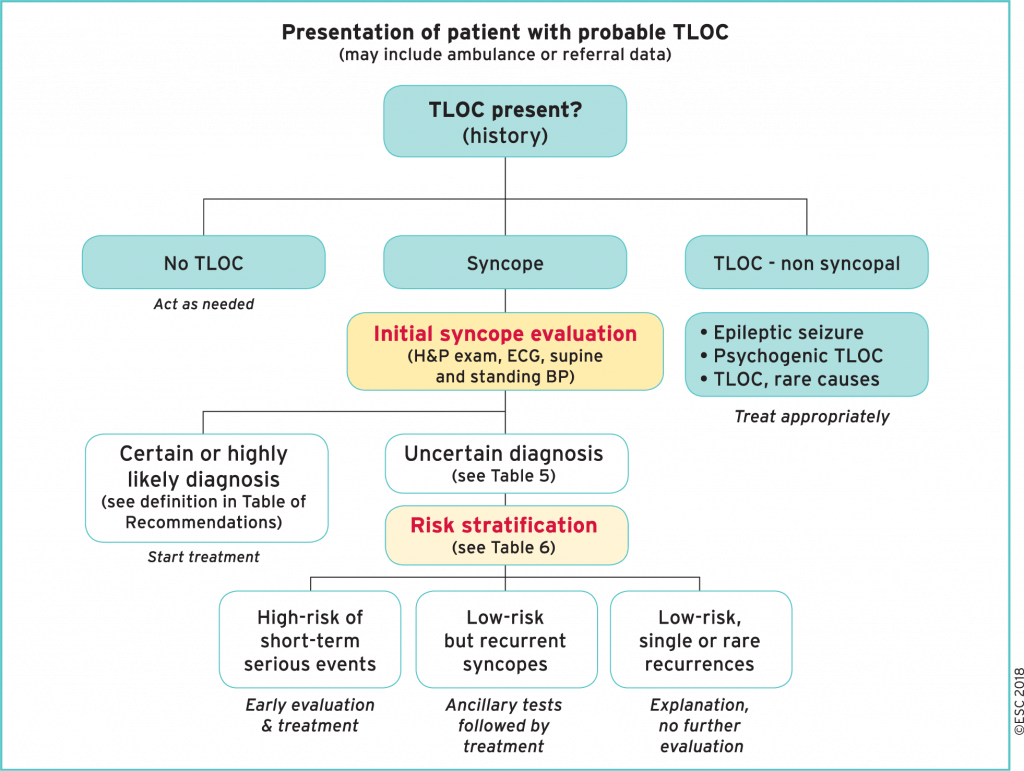
Diagnostic Approach
Initial Evaluation
- Determine if true loss of consciousness/syncope and rule out other causes: seizure, psychogenic, etc
- Gather history from witnesses (where possible)
- Physical exam, including supine and standing blood pressure (see orthostatic challenge below)
- ECG
- Blood tests (hemoglobin, electrolytes, etc.)
History
- It is crucial to take a detailed history from the patient, and any witnesses to help come to a diagnosis. Below are listed low and high-risk features of syncope.
- Questions to consider asking:
- What’s the last thing you remember?
- Did you have a chance to brace yourself?
- Did you know something was about to happen?
Low Risk:
- Associated with prodrome (light-headedness, warmth, nausea, vomiting)
- After sudden unexpected sensation (sound, smell, pain)
- Associated with prolonged standing
- During a meal or post prandial
- Triggered by cough, defecation, or micturition
- Occurring with head rotation
- Standing from supine/sitting position
- Recurrent history
High Risk:
- New onset of chest pain/discomfort, dyspnea, headache
- Syncope when supine or during exertion
- Sudden onset of palpitation preceding syncope
- No warning or prodrome
- Family history of sudden cardiac death at young age
- Syncope in sitting position
- Severe structural or coronary disease
Physical Exam
- General exam, to rule out consequences of trauma and a cardiac exam is needed to help determine whether structural causes are present.
- Orthostatic Vitals
Low Risk:
- Normal Examination
High Risk:
- Unexplained systolic BP <90mmHg
- Persistent Bradycardia <40bpm when awake and absence of physical training
- Undiagnosed systolic murmur
ECG
- Bifascicular block (defined as either left or right BBB combined with left anterior or left posterior fascicular block)
- Other intraventricular conduction abnormalities (QRS duration >0.12 s)
- Mobitz I second-degree AV block and 1-degree AV block with markedly prolonged PR interval
- Mobitz II second degree and third-degree heart block
- Asymptomatic mild inappropriate sinus bradycardia (40–50 b.p.m.) or slow atrial fibrillation (40–50 b.p.m.) in the absence of negatively chronotropic medications
- Non-sustained VT
- Paroxysmal A.Fib or SVT
- Pre-excited QRS complexes
- Long or short QT intervals
- Early repolarization
- ST-segment elevation with type 1 morphology in leads V1-V3 (Brugada pattern)
- Negative T waves in right precordial leads, epsilon waves suggestive of ARVC
- Left ventricular hypertrophy suggesting hypertrophic cardiomyopathy
Special Tests
Orthostatic Challenge
- Should be performed in anyone presenting with syncope.
- Diagnostic criteria: Abnormal BP fall is defined as a progressive and sustained fall in systolic BP from baseline value >20 mmHg or diastolic BP >10 mmHg, or a decrease in systolic BP to < 90 mmg Hg.
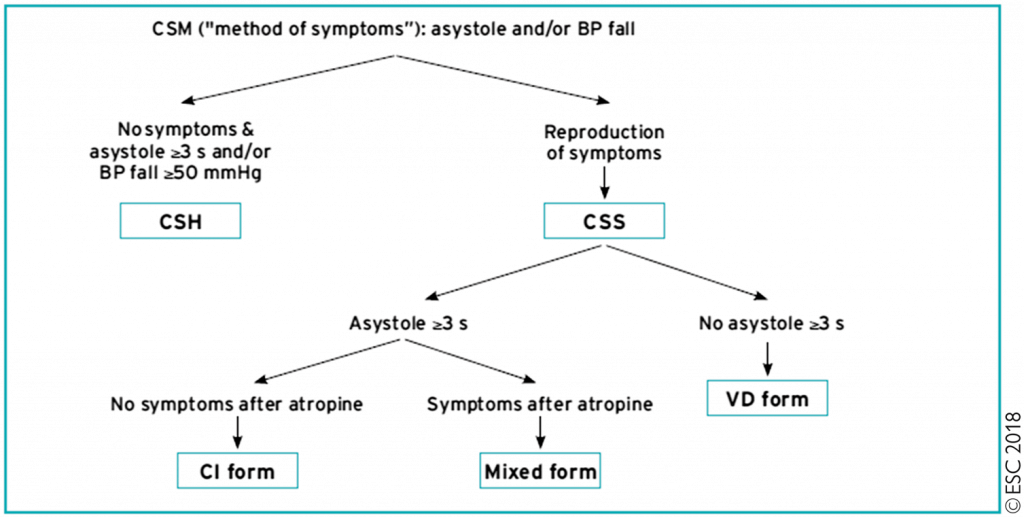
Carotid Sinus Massage
- Can be performed in individuals above the age of 40 (carotid sinus hypersensitivity is quite common in younger individuals).Cardioinhibitory CSH was defined as asystole of 3 seconds or more with a drop in SBP of less than 50 mm Hg (vasodepression). Specificity increases with age and if syncope recurs with carotid sinus massage.
- Carotid sinus syndrome is diagnosed if the above test reproduces syncope/pre-syncope. This is usually in patients with syncope suspected to be due to a reflex mechanism.
- How to perform the test: Click here
Cardiac Evaluations
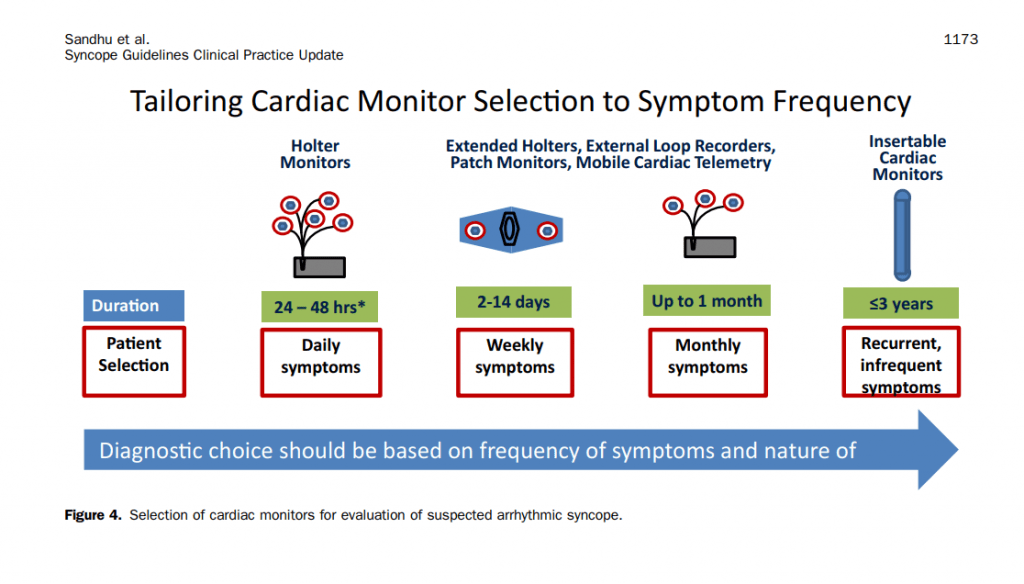
Electrocardiographic Monitoring
- ECG monitoring is indicated if there is high suspicion for an arrhythmogenic cause (see ECG section above).
- Correlation between symptoms and ECG recording is the gold standard for diagnosis cardiac syncope.
- Immediate in-hospital monitoring is indicated (ie. telemetry) in high risk patients.
- Low risk patients managed as an outpatient, the decision depends on frequency of events to determine length of monitoring needed (ie. several days with a holter vs several months with an implantable loop recorder).
Echocardiography
- Indicated in patients when there is previous known heart disease, data suggestive of structural heart disease, or syncope secondary to cardiovascular cause
Exercise Stress Testing
- Indicated in patients with syncope during or shortly after exertion
Outpatient monitoring
Neurologic Evaluation
Brain imaging
- Should be performed only for patients for whom intracranial disease is highly suspected as a possible contributing cause to syncope, or if there has been a suspicion of head trauma as a result of syncope.
Carotid artery imaging
- Should not be performed routinely (in the absence of neurological symptoms)
Diagnosis
- Click here for clinical features that can suggest a diagnosis on initial evaluation by ESC
- ESC Class 1 Recommendations
Reflex and Orthostatic
- Vasovagal syncope is highly probable if syncope is precipitated by pain, fear, or standing, and is associated with typical progressive prodrome (pallor, sweating, and/or nausea).
- Situational reflex syncope is highly probable if syncope occurs during or immediately after specific triggers (see above).
- Syncope due to OH is confirmed when syncope occurs while standing and there is concomitant significant OH.
- In the absence of the above criteria, reflex syncope and OH should be considered likely when the features that suggest reflex
syncope or OH are present and the features that suggest cardiac syncope are absent (see above list).
Cardiac
- Arrhythmic syncope is highly probable when the ECG shows
- Persistent sinus bradycardia <40 b.p.m. or sinus pauses >3s in awake state and in absence of physical training;
- Mobitz II second- and third-degree AV block;
- Alternating left and right BBB;
- VT or rapid paroxysmal SVT;
- Non-sustained episodes of polymorphic VT and long or short QT interval;
- Pacemaker or ICD malfunction with cardiac pauses.
- Cardiac ischaemia-related syncope is confirmed when syncope presents with evidence of acute myocardial ischaemia with or without myocardial infarction.
- Syncope due to structural cardiopulmonary disorders is highly probable when syncope presents in patients with prolapsing
atrial myxoma, left atrial ball thrombus, severe aortic stenosis, pulmonary embolus, or acute aortic dissection.
Management
Risk Stratification
- Consider using validated risk score to triage patients though none shown to be better than clinical judgement
- ESC proposed triage for admission vs discharge:
General Approach
- Further management should be direct based on above evaluation to confirm diagnosis
- Once diagnosis confirmed, management should be instituted accordingly (ie. complete heart block –> recommend pacemaker)
Reflex Syncope
- Education and lifestyle modifications is mainstay of treatment (Class I)
- Reassurance of benign condition
- Recognition of prodrome to order to sit/lie down and activate counterpressure manoeuvres
- Manoeuvers include squatting (best), leg crossing, tensing abdo/leg muscles
- Avoid triggers: Cough suppression in cough induced syncope, micturition in the sitting position, avoiding crowded places, etc.
- Increased intake of oral fluids (Class IIB Indication)
- Limited evidence, unclear long-term effects
- Avoid in HTN, CKD, HF
- 2-3L fluid/d, 6-8g of salt/day (1-2 tea spoons)
- Discontinue/reduce hypotensive therapy
- Pharmacologic Therapy (2nd line)
- Midodrine (Class IIA)
- Alpha-agonist, causes vasoconstriction
- Best Data: Meta-analysis of 5 RCTs –> 43% reduction in recurrent VVS
- Avoid in HF, HTN, Urinary Retention
- Fludrocortisone (Class IIB)
- Causes salt/water retention & K+ excretion, increased blood volume
- POST II Trial – 31% improvement in recurrent VVS
- Better for younger patients with low BP
- Midodrine (Class IIA)
- Other Therapy
- B-Blockers if ≥ 42yo (Class IIB)
- SSRI (Class IIB)
Note: VVS = Vasovagal Syncope
Orthostatic Syncope
- Education and lifestyle measures,as above in reflex syncope (Class I ESC)
- Acute water ingestion for temporary relief (Class I AHA)
- Effect seen 30min after ≥ 240mL
- Adequate hydration and salt intake (Class I ESC, Class IIB AHA)
- Targeting 2–3 L of fluids per day
- 10 g of sodium chloride
- Rapid ingestion of cool water can be effective in combating orthostatic intolerance and postprandial hypotension.
NOTE AHA Guideline classifies as Class IIB due to unknown long term effects from high salt ingestion
- Discontinuation/reduction of vasoactive drugs (Class IIa ESC)
- Counterpressure manoeuvres (Class IIa)
- Leg crossing, lower-body muscle tensing
- Squatting (best)
- Only helpful if adequate prodrome
- Abdominal binders and/or support stockings (Class IIa)
- Head-up tilt sleeping (Class IIa – ESC)
- Pharmacological (Class IIa):
- Midodrine: Dosage (2.5–10 mg t.i.d) was shown to be effective in some RCTs (monitor for supine hypertension, urinary retention)
- Fludrocortisone (Observational Data) in conjunction with head-up tilt sleeping
- Considered 2nd line by AHA 2017
- Droxidopa for neurogenic OH (Class IIA AHA)
- Esp. effective for parkinson’s disease
- Pyridostigmine can be considered in refractory neurogenic orthostatic hypotension (OH), and Octreotide has been used in post-prandial OH (Class IIB AHA)
Role of permanent pacemaker
- Orthostatic Syncope –> Generally no role for PPM
- Vasovagal Syncope –> May be a role for PPM (see below)
- There are two components of vasovagal syncope:
- vasodepressor response (which causes vasodilation + hypotension)
- cardioinhibitory response (which causes bradycardia/pauses + reduced cardiac output)
- A permanent pacemaker (PPM) improves the heart rate during times of VVS, however it does not treat the vasodilation and hypotension.
- Major Trials:
- VPS I Trial: Randomized pacing vs no pacing in patients with recurrent VVS. Group with PPM had fewer symptoms. This trial was criticized because it was not blinded.
- VPS II Trial: Landmark trial included 100 patients with recurrent drug-refractory VVS. Investigators implanted pacemakers in all patients. Patients were randomized in a blinded fashion to no pacing (device programmed to no pacing) vs. pacing.
- There is no significant difference in symptoms between pacing and no-pacing arms.
- Demonstrates the power of placebo in VPS 1 trial.
- Many patients still had syncope due to hypotension/vasodilation component.
- Conclusion:
- New CCS guidelines recommended below (based on AHA and ESC recommendations)
- Patients 40 years of age or older with highly symptomatic recurrent VVS might benefit from dual-chamber pacing if they have either:
- Documented symptomatic asystole > 3 seconds or asymptomatic asystole > 6 seconds; or
- Tilt-induced: asystole > 3 seconds or heart rate < 40 beats per minute for > 10 seconds.
- The patient should be seen urgently (within 2 weeks) by a cardiologist/electrophysiologist depending on the local practice to review results, decision regarding management, and arrange next steps for implantation, if needed.
- Permanent pacing can be considered in select patients > 40yo with recurrent VVS and prolonged spontaneous pauses (AHA Class IIB)
- Must weigh risks of pacemakers (lifetime risk of infection/endocarditis, generator changes, perforation, pneumothorax etc.) vs. benefit
- Reserved generally for patients with cardioinhibitory (pauses) syncope, and less vasodepressor component
- Clinicians must be familiar with driving guidelines related to syncope.
- Please review the CardioGuide Driving Guidelines summary (CMA/CCS Recommendations)
- There are two components of vasovagal syncope:
Cardiac Syncope
- Management depends on pathology, for example pacemaker/ICD for arrhythmia and surgical consideration for aortic stenosis
- For more information on management of cardiac syncope and indications for cardiac implantable device, see topic Cardiac Syncope Management, Aortic Stenosis, Hypertrophic Cardiomyopathy
Further Reading
Authors
- Primary Author: Dr. Dimitar Saveski (MD, FRCPC, Internal Medicine Resident)
- Author/Reviewer:
- Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Pavel Antiperovitch (MD, FRCPC)
- Staff Reviewer: pending (MD, FRCPC[Cardiology])
- Last Updated: August 28, 2020
- Comments or questions please email feedback@cardioguide.ca