Introduction
- Prerequisite Reading: Narrow QRS Tachycardia
- NOTE: The term “SVT – Supraventricular Tachycardia” refers to narrow-QRS regular tachycardia. Even though atrial fibrillation is “supraventricular”, it is not an SVT.
| Narrow QRS Regular Tachycardia |
|
Tips
Locating P-waves
- A QRS complex can take many shapes and forms. Never call a P-wave within a QRS complex.
- P-waves are SHARP (high-frequency) deflections. They are always sharper than T-waves. If you see a high-frequency deflection in a T-wave, it is likely a P-wave!
- Template the T-wave in sinus rhythm to the T-wave in the tachycardia. If it appears different, there may be a superimposed P-wave.
- Often times no reliable P-wave can be identified. This is ok – it is better to recognize this and have a differential diagnosis than overcall it.
ECG Characteristics that are NOT helpful:
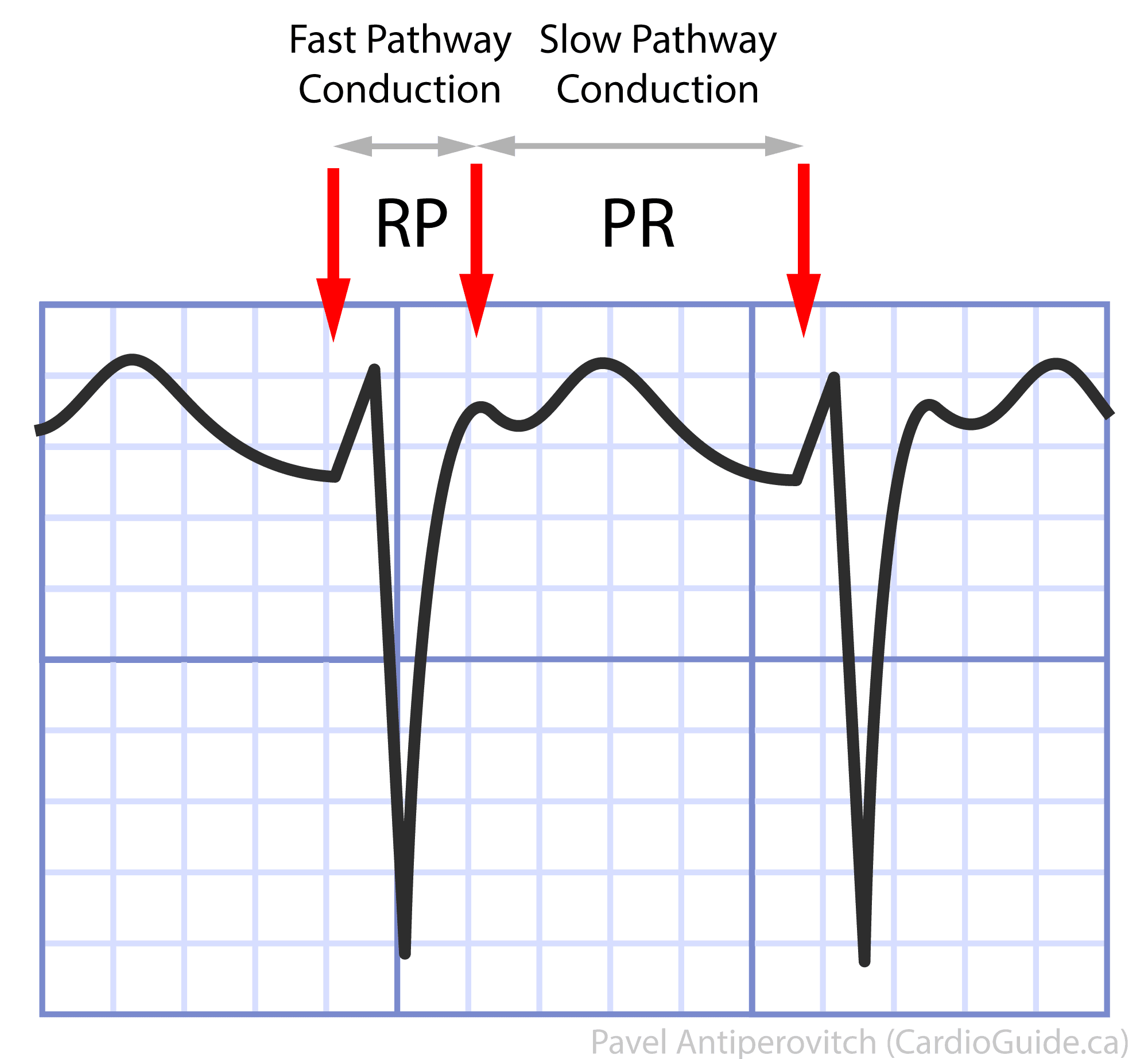
- Long RP / Short RP
- Can be highly variable depending on the response of the AV node.
- A “short-RP” tachycardia is often characterized by RP<PR, which translates to a short V-A and long A-V time. It can be atrial tachycardia with a 1st degree AV block (delay in the AV node during tachycardia), sinus tachycardia with a 1st degree AV block, typical slow-fast AVNRT, and orthodromic AVRT.
- A “long-RP” tachycardia that has RP > PR can be an atrial tachycardia, fast-slow “atypical” AVNRT, and AVRT with a slowly-conducting pathway.
- Both classifications have the same differential diagnosis list.
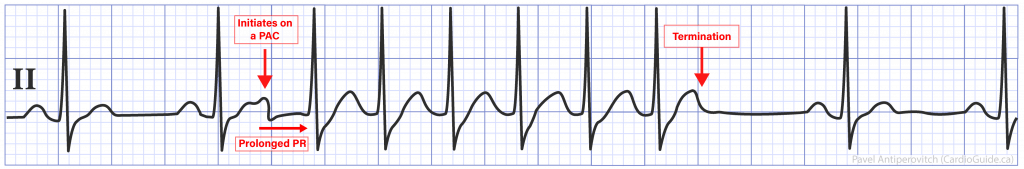
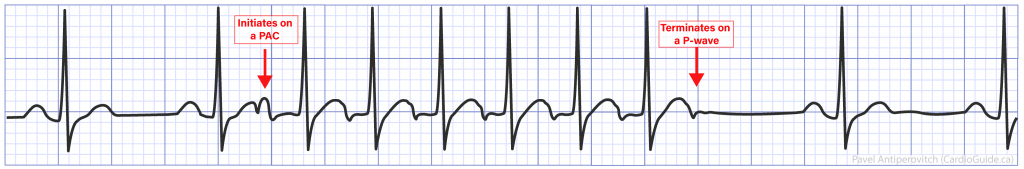
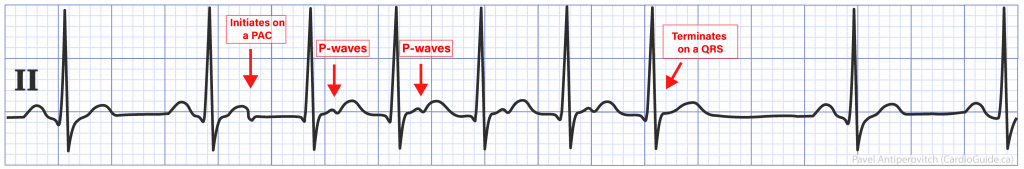
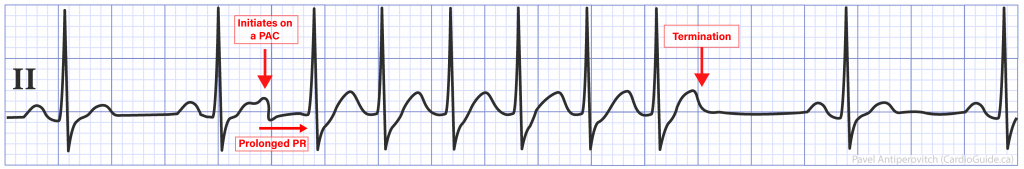
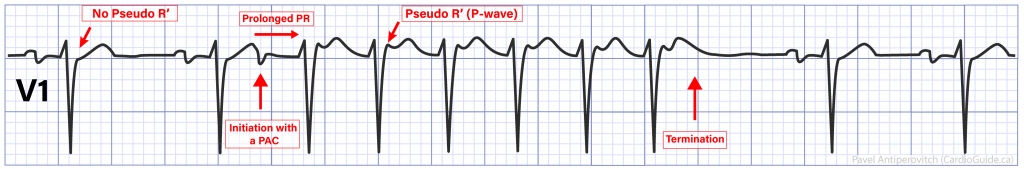
- Initiation with a PAC with a long PR interval
- Initiation with a PAC helps rule-in SVT and rule out VT, but does not help in the differential diagnosis of SVT.
- Most SVTs start with a PAC, with is an early atrial activation before next scheduled sinus beat. Most PACs cause an AV conduction delay, where the AV node decrements in response to a long-short sequence.
- QRS alternans (alternating amplitude of the QRS) has been classically described in AVRT, but has been shown to be present in any fast SVT
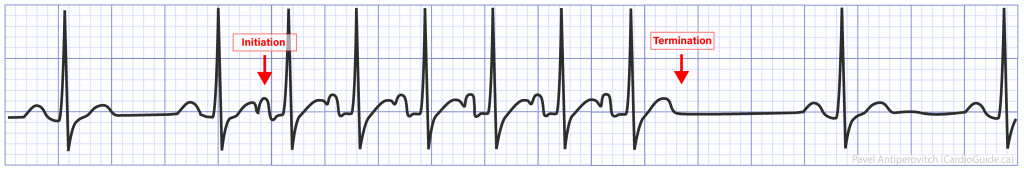
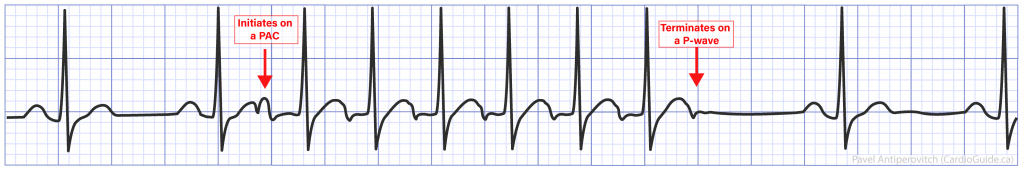
Initiation & Termination
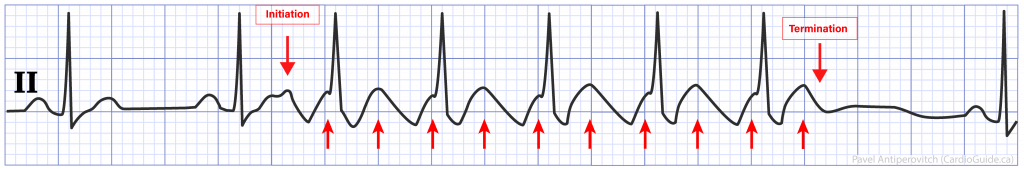
- Initiation on a PAC with PR prolongation
- Required for Typical AVNRT
- AT can initiate on PAC, but does not require PR prolongation (NOTE: PR can lengthen after any PAC due to the decremental property of the AV node)
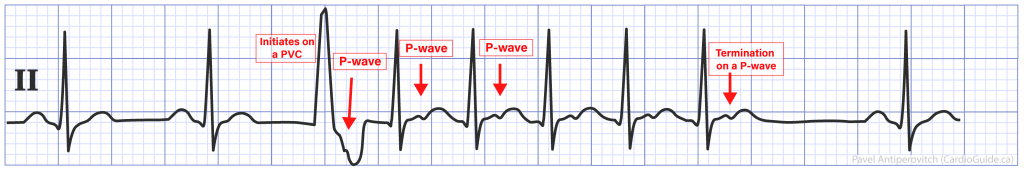
- Initiation with a PVC
- Most commonly a trigger AVRT, and sometimes atypical (fast-slow) AVNRT
- AVRT: PVC can activate the atrium through the accessory pathway, and unable to conduct retrograde up the AV node. The activated atrium then conducts anterograde through the AV node to activate the ventricles.
- Atypical AVNRT: PVC can conduct retrograde up the AV node, finds slow pathway refractory (from late activation), and activates the atrium via fast pathway, which can then re-enter via slow pathway.
- Atypical AVNRTs are rare, so AVRT is higher on the differnential.
- Rarely triggers typical AVNRT and it is extremely rare for AT.
- Most commonly a trigger AVRT, and sometimes atypical (fast-slow) AVNRT
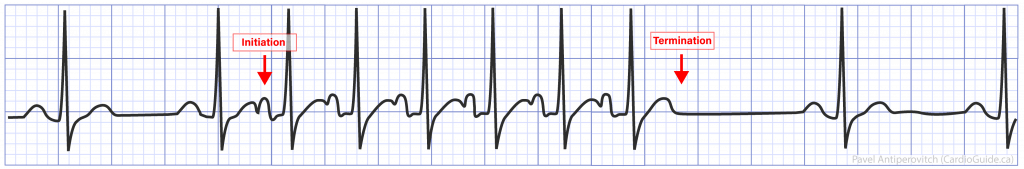
- Termination on a P-wave
- Rules out AT (To explain this with AT, the arrhythmia must terminate, and at the same time have an AV block. Both of these events are extremely unlikely to happen simultaneously)
- NOTE: Termination on a QRS (no p-wave) is not helpful
Changes in Cycle Length
- When there is a change in cycle length, measure out the intervals to see what happens first (does the A move, and V follows? or opposite?)
- Atrial cycle length changes first (“A’s leading the V’s”)
- AT and atypical AVNRT (A–>V interval is fixed by fast pathway)
- Ventricular cycle length changes first (“V’s leading the A’s”)
- Typical AVNRT or AVRT
- Excludes AT
RP Interval
- Very short RP interval (< 90ms) and VA interval (≤ 70ms on EP study)
- Indicates typical AVNRT (or less commonly focal AT)
- Generally excludes AVRT (signal must travel through ventricles before re-entering the atrium through accessory pathway, which takes > 70ms, but rare exceptions reported)
- A “longer” RP interval > 90ms
- Excludes typical AVNRT (absence of fast pathway)
- Possibilities: AT, AVRT, and Slow-Slow AVNRT
- of those possibilities, AVRT is most common, followed by AT, and slow-slow AVNRT is extremely rare.
P-wave Morphology
- P-waves similar to those in sinus rhythm
- Supports ST, AT with focus close to the sinus node, and Sino-atrial re-entry tachycardia (atrial activation re-enters the sinus node through a connection, and activates the atrium again)
- P-waves different than sinus rhythm –> Rules out above
QRS Morphology
- If QRS is wide ≥ 120ms, see post on “Wide QRS Tachycardias”
- Compare the QRS in tachycardia to the QRS in sinus rhythm!
- New pseudo-R’ in V1 and pseudo-S in inferior leads
- More common in typical AVNRT, than AVRT or AT.
- In AVNRT, the fast pathway creates a short RP interval, and often retrograde P-wave is buried in the terminal portion of QRS.
- QRS notch in aVL and pseudo-r in aVR have been shown to be be more sensitive+specific for AVNRT than V1. (Haghjoo et al Europace 2012)
Other
- AV Dissociation
- Rules out AVRT (both atria are ventricles are required to complete the circuit)
- Development of Bundle Branch Block (BBB) during arrhythmia
- If BBB is ipsilateral to AP, can result in prolongation of cycle length (signal must travel around blocked bundle to get to the pathway)
- The Rate
- Generally not helpful as none of these mechanisms require a certain rate.
- The only excpeion is rate of ~150bpm. Atrial rate in atrial flutter is typically ~300bpm, so a 2:1 AV block produces a ventricular rate of ~150bpm. However, the circuit can be slowed if the patient receives an anti-arrhythmic, and all bets are off!
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
The Mechanisms
Sinus Tachycardia (ST)
- Involves increased automaticity of the SA node
- ECG Characteristics:
- Gradual onset & offset (driven largely by the autonomic nervous system)
- P-wave morphology matches P-waves in sinus rhythm
- [Should originate in the SVC-RA junction –> positive P-waves in inferior leads (II, III, aVF) and left-ward leads (I and aVL)]
- Presence of medical conditions that drives ST (sepsis, Inotropes/pressors, dehydration)
- Response to adenosine:
- Gradual slowing of the tachycardia and then re-acceleration
- Management:
- Identify underlying disorder
- Correct the underlying disorder
- Generally rate control is not indicated
Focal Atrial Tachycardia (AT)
- Automaticity of focal site in the atrium.
- NOTE: The term “Atrial Tachycardia (AT)” is often used to describe tachycardias arising in the atrium (Sinus, Focal Atrial Tachycardia, Atrial Flutter), > 150 bpm, when mechanism is not known.
- ECG Features to Rule In:
- P-waves often have different morphology to sinus P-waves
- Caveat: P-wave morphology can match sinus P-waves when the focus is close to the sinus node.
- P-wave morphology can resemble retro-conducted P-waves if the origin is close to the AV node.
- P-waves often have different morphology to sinus P-waves
- ECG Features to Rule Out:
- SVT that terminates on a P-wave is significantly less likely to be AT
- Explanation: If a tachycardia terminates on a P-wave, the atrial focus must stop firing, and the AV node must block on the same beat. Both of these events are unlikely to happen on the same beat, hence this makes AT a lot less likely
- Sometimes a “Warm-Up” and “Cool-Off” phenomenon can be seen where the tachycardia accelerates and gradually slows down before terminating.
- SVT that terminates on a P-wave is significantly less likely to be AT
- Response to adenosine:
- Adenosine blocks the AV node, which stops ventricular activation, revealing AT P-waves. Compare these P-waves to the sinus ECG.
- Tachycardia continues after adenosine effect wears off.
- NOTE: Some atrial tachycardias are adenosine-sensitive, and can slow down or terminate with adenosine.
- NOTE: AT is very difficult to exclude in an SVT because P-waves can take any shape or form depending on the AT origin. AV nodal conduction can slow, which can lengthen the PR interval and place the P-wave anywhere in the tachycardia cycle.
Management:
- Acute Management:
- Can give adenosine for diagnostic clarity, but it generally does not break the tachycardia.
- Cardioversion can be attempted, but many are resistant to this.
- Anti-arrhythmics (Amiodarone or Class IC agents)
- Chronic Management
- Anti-arrhythmics
- Catheter ablation – often difficult because AT can only be mapped and ablated when the patient is in this rhythm.
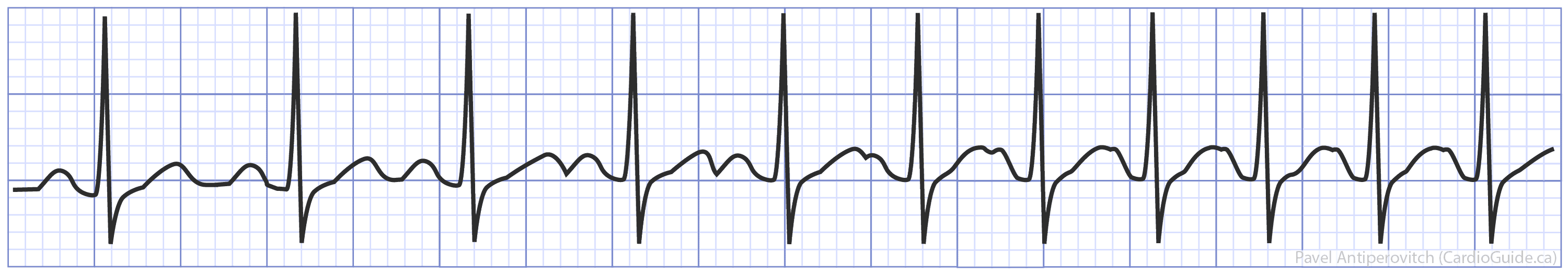
Atrial Flutter
- Type of atrial tachycardia where there is a macro-reentry circuit around the IVC. The narrowest part of the circuit is the space between the IVC and Tricuspid Annulus [called Cavo-Tricuspid Isthmus (CTI)]
- ECG Features:
- “Saw-tooth” pattern in inferior leads.
- Rate of 150bpm raises the likelihood of atrial flutter.
- Classic rate of atrial flutter circuit is 300bpm. Fortunately, the AV node usually cannot conduct this quickly, and introduces a 2:1 block, which makes the QRS rate 150bpm.
AV Nodal Reentry Tachycardia (AVNRT)
- Involves a macro-reentry circuit in the AV node.
Pathology:
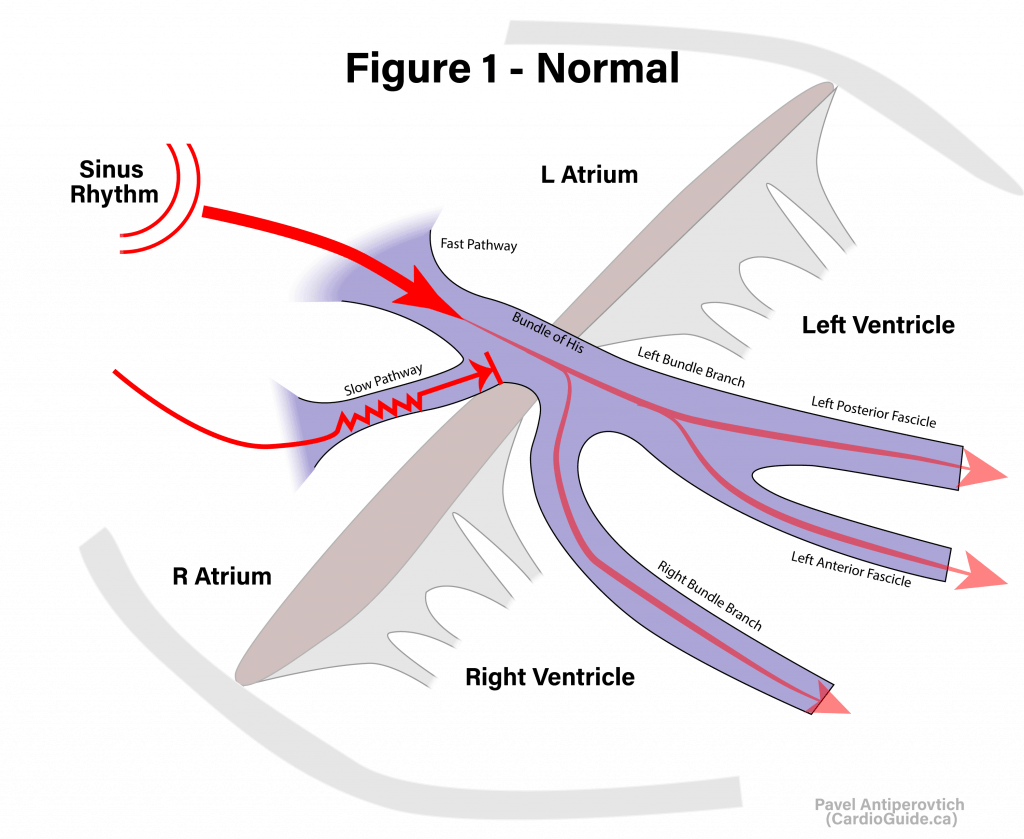
- Normal AV nodal tissue has two entry points:
- Fast Pathway: Conducts quickly and has a long recovery time (long refractory period).
- Slow Pathway: Conducts slowly, and has a short recovery time (short refractory period).
- Under normal circumstances, the fast pathway predominates, and by the time the slow pathway reaches the common fibres, the fast pathway already activated them, and the activation in the slow pathway terminates (Figure 1).
Slow-Fast “Typical” AVNRT: On occasion, a specially-timed PAC can reach the AV node at a vulnerable time period, such that the fast pathway is refractory. It then enters the node via the slow pathway (Figure 2). By the time it reaches the common fibres, the fast pathway recovers. The signal goes down to activate the ventricles, and at the same time retro-conducts up via fast pathway to the atria, which activates the slow pathway again resulting in a macro-reentry circuit. This is slow-fast “typical” AVNRT.
Fast-Slow “Atypical” AVNRT is a variation where signal goes down the fast pathway to activate the ventricles, and retro-conducts up the slow pathway to activate the atria (opposite). The P-wave preceeds the QRS complex. This type is also very uncommon.
Slow-Slow AVNRT is possible where both pathways are slow, but one is slower with a longer refractory period (very rare!). The P-wave can be anywhere between the two QRS complexes depending on the relative conduction velocity in the two pathways.
ECG Features:
- Retrograde P-waves (negative in inferior leads [II/III/aVF], terminal positive component in V1).
- Pseudo-R‘
- P-waves in AVNRT are often not visible because they are fused with the terminal portion of the QRS (Figure 4)
- However, you can see the P-wave affecting the termination portion of the QRS in lead V1 by the presence of an R’ that was not there before (Figure 6).
- To confirm, you must compare the QRS in tachycardia to the QRS in sinus rhythm (Figure 6)
- Generally starts on a PAC with a long PR interval (represents conduction in the slow pathway), but this doesn’t help distinguish SVTs.
AV Re-Entrant Tachycardia (AVRT)
- A macro-re-entry circuit that involves the AV node and an accessory pathway.
- ECG Features to Rule In:
- Initiates on a PAC or PVC