Introduction
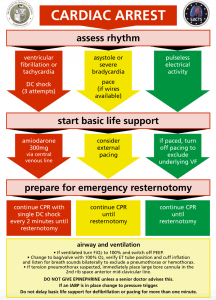
- Resuscitation in patients who have had cardiac surgery differs from traditional ACLS.
- Patients often have unique causes of the arrest related to surgical complications.
- The incidence of arrest is 0.7-8% following cardiac surgery.
- Unlike most cardiac arrests – cardiac arrest following cardiac surgery often have better outcomes in terms of return of spontaneous circulation (ROSC) and neurological outcome.
- Prompt recognition and management is critical by both the ICU and cardiac surgery teams.
Etiology
- VF arrest accounts for 25-50% of the cardiac arrests.
- Cardiac tamponade and other major bleeding account for large portion of other cardiac arrests.
Key Differences
- Emergency re-sternotomy is a critical component of cardiac arrest management.
- Emergency re-sternotomy is a part of standard of care up until they leave ICU or 10 days post cardiac surgery. Beyond 10 days it can still be considered but generally senior clinician should decide. At 10 days and beyond there is a risk of adhesions – though late tamponade is still possible especially if recent epicardial wire removal or anticoagulation use.
- Of note: these guidelines apply to patients undergoing sternotomy operations and does not apply to other types of procedures (e.g. minimally invasive procedures, patients supported by ECMO/LVAD).
Defibrillation/pacing
- Unlike traditional ACLS – if VF/Pulseless VT is identified it is recommended that 3 shocks be attempted before CPR.
- Traditionally asystole is managed with a general PEA algorithm. However, in post cardiac surgery patients given intrinsic conduction system can be damaged – pacing should first be attempted.
- If paced PEA arrest -> turn off to exclude VF.
This algorithm suggest delaying CPR for initial management. The reason for this is recent sternotomy and the risk of life threatening bleeding with CPR. Can delay for 1 minute while troubleshooting cardiac arrest before initiating CPR.
Clinical Pearls
- Inability to get a systolic pressure of over 60mmHg -> suggest severe bleeding or tamponade.
- Although an uncommon cause of cardiac arrest in cardiac patients -> always consider tension pneumothorax. Consider needle decompression, finger thoracostomy, check that the chest tubes are patent, attached to the chest drains and are on to suction.
- Giving full dose cardiac epinephrine should only be done if instructed by senior clinician. Risk of severe hypertension and worsening bleeding if ROSC is achieved.
- IABP – can trigger based on EKG or pressure. In cardiac arrest this mode should be switched to pressure mode in order to help facilitate CPR. If CPR is being held for emergency sternotomy can set the IABP to internal mode usually at a rate of a 100.
- Internal cardiac massage is preferred over external and has better evidence for better coronary perfusion and successful ROSC.
- Abdominal compressions can be considered when performing emergency sternotomy given the inability to do CPR at that time.
Emergency Sternotomy
In non-VF/VT arrest the most common cause is cardiac tamponade. If ROSC does not occur with pacing and ruling out other immediate causes, emergency re-sternotomy should be performed as soon as possible and at least within 5 minutes of cardiac arrest.
Consider cooling protocol as per standard AHA guidelines.
- All cardiac ICU’s should be equipped with an emergency re-sternotomy kit.
- Generally the kit only needs 5 things: a sternal retractor, scalpel, wire cutter, needle holder, and suction.
- More complex kits can be developed but this risks confusing less skilled person not familiar with procedure.
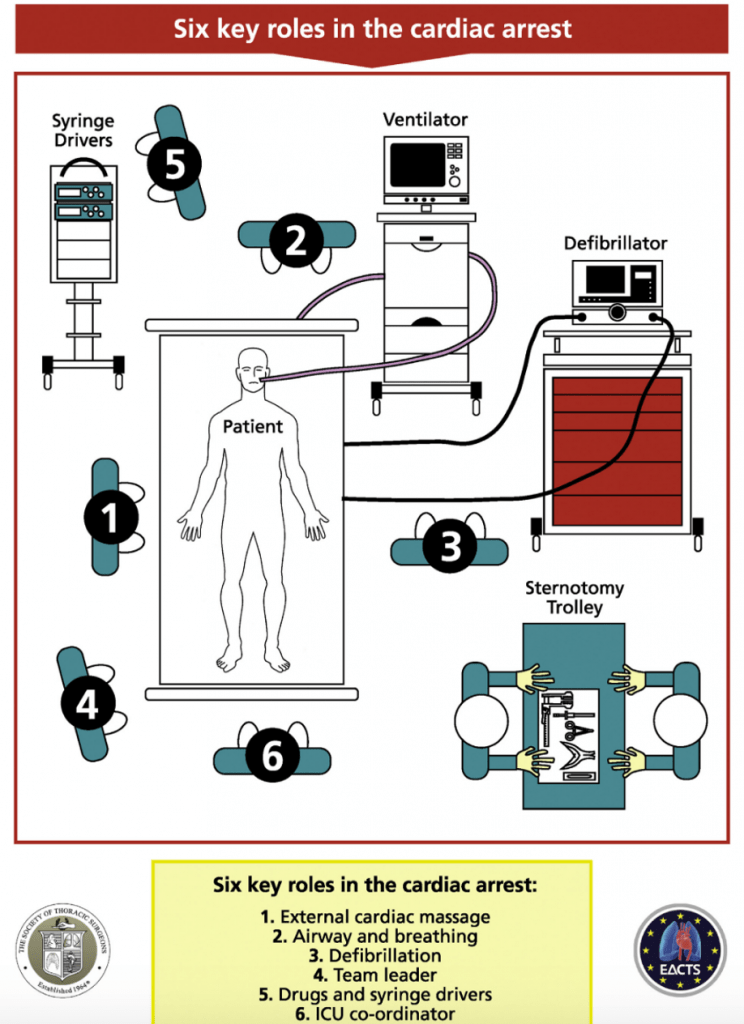
- Generally at least two team members should be tasked with the re-sternotomy.
- It is good practice to remain as sterile as possible.
- The most experience with the operation should be performing the emergency re-sternotomy but waiting for more senior personal can be fatal and the procedure should be done ideally within 5 minutes of cardiac arrest refractory to defibrillation, CPR, medications, and pacing.
- Usually the quickest way to open the chest is to have one person cutting the sternal wires and the other pulling them out.
- Once the chest is open internal cardiac massage can be performed by experienced clinicians.
Further Reading
The Society of Thoracic Surgeons Expert Consensus for the Resuscitation of Patients Who Arrest After Cardiac Surgery. https://www.sts.org/sites/default/files/documents/ExpertConsensus_ResuscitationAfterCardiacSurgery.pdf
Authors
- Authors: Dr. Daniel Durocher (MD, FRCPC, Cardiologist and ICU Fellow)
- Staff Reviewer: Dr. Julian Owen (MD, FRCPC, Emergency Medicine/Critical Care)
- Last Updated: August 26, 2021
- Comments or questions please email feedback@cardioguide.ca