Introduction
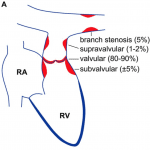
- Pulmonary stenosis is relatively common occurring in 7% of children with congenital heart disease
- Multiple types of pulmonary stenosis include, valvular (most common), subvalvular, and supravalvular
- Pulmonary stenosis is most commonly congenital but may be acquired
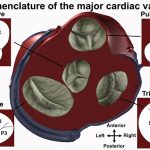
Anatomy
- Pulmonary valve is anterior and elevated by the infundibulum (or RVOT) to be superior to the aortic valve, locating it above the ventricular septum
- Similar to the left side, the pulmonary root has 3 sinuses of valsalva formed by the attachments of three semilunar leaflets
- Valve nomenclature is based on the aortic valve, thus the two valves bordering the septum are known as the left and right leaflets (corresponding to the AV) and the third is anterior (or non-coronary leaflet)
- In pulmonary stenosis valve can uncommonly have 1-2 leaflets and rarely 4 leaflets.
Diagnosis
Clinical
- Physical exam: systolic ejection murmur LUSB, split S2, right sided S4, prominent A wave, RV heave
- Mild PS rarely symptomatic and generally not progressive
- Moderate PS can be progressive and Severe PS can cause decreased exercise tolerance and shortness of breath.
- In severe stenosis, the right heart cannot augment cardiac output, thus can have chest pain, syncope or sudden cardiac death
- Right heart failure uncommon but can occur if severe PS is left untreate
Multi-Modal Imaging
- Cardiac CT: useful in assessing anatomy, especially pulmonary arteries which are difficult to assess on echo and in patients with foreign material (valve replacement, pacemakers etc)
- Cardiac MRI: Useful in assessing PR and RV size and function
- Cardiac catheterization: Directly measure gradient. Severe PS is defined by gradient > 60mmHg
Echocardiography
- TTE evaluation of the pulmonary valve is limited in adults by body habitus and previous interventions
- TEE can be used though also not optimal as probe posterior and valve is anterior
- Beyond scope of this talk but more information in the references
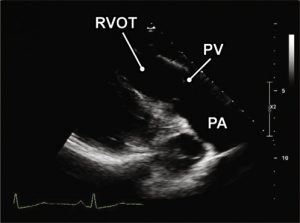
Echocardiographic Views
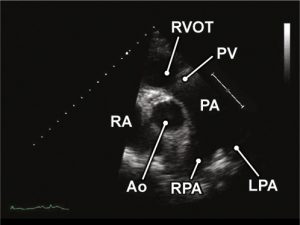
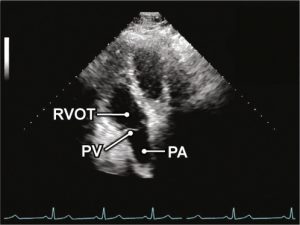
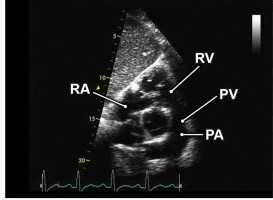
- RVOT/PV/PA
- PLAX, PSAX, A5C, Subcostal Short Axis
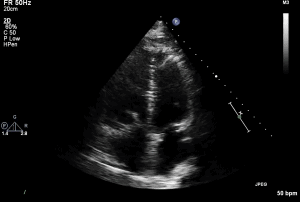
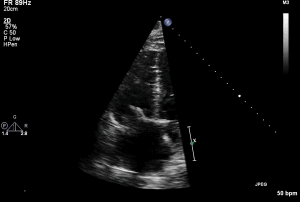
- RVH
- PLAX and Subcostal Long Axis
- RV Dilation
- Apical 4 Chamber
- RV Function
- Difficult by TTE
RVOT Views (ASE):
1 PLAV RVOT
2 PSAX RVOT
4 A5C RVOT
5 Subcostal RVOT
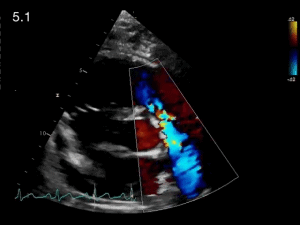
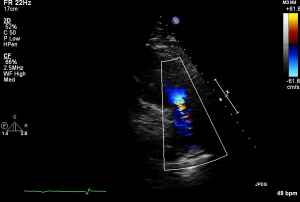
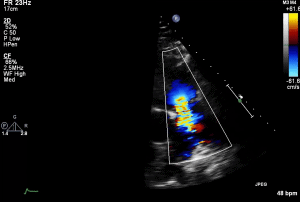
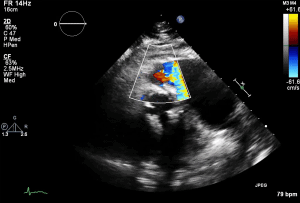
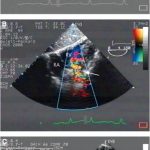
PSAX RVOT Colour
Echocardiographic Diagnosis
- Goals are to assess location of obstruction, valve morphology and degree of stenosis
- In addition looking for associated findings such as right ventricular size and function, RVOT and PA anatomy
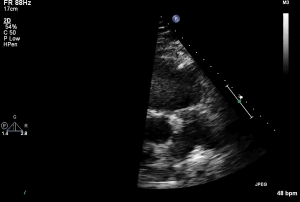
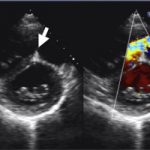
- 2D Imaging
- Assess valve for thickened leaflets, doming, calcifications (uncommon)
- Post-stenotic dilation of MPA
- RV size is usually normal
- RV hypertrophy (>5mm)
- Colour flow doppler:
- turbulence/aliasing (maximum area of turbulence to determine site of stenosis)
- Pulmonary regurgitation
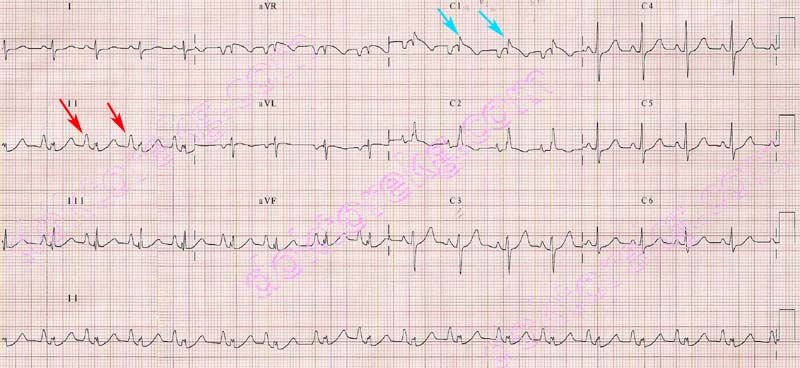
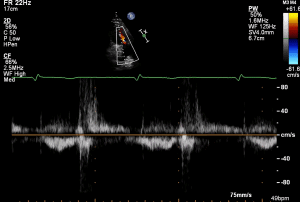
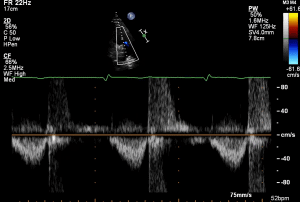
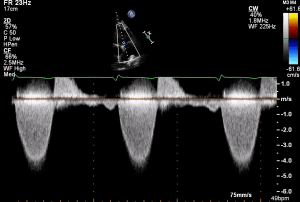
- Doppler
- PW doppler to localize peak site of velocity
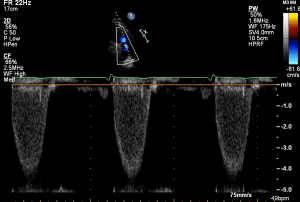
- CW doppler
- peak velocity/VTI
- mean gradient
- peak gradient (4v^2)
- Average 3-5 cycles to adjust for respiratory changes
- Grading severity
- Quantitative evaluation
- PV area not validated and planimetry difficult
- Need multiple views and use highest CW velocity
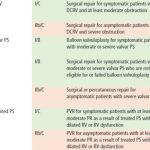
| Mild | Moderate | Severe | |
| Peak Velocity (m/s) | <3 | 3-4 | >4 |
| Peak gradient (mmHg) | <36 | 36-64 | >64 |
Valvular
- Congenital
- Almost always congenital in origin and commonly with associated defects
- Classically domed or conical structure without separation of cusps and small central orifice
- On echo appears as mildly thickened leaflets with restricted systolic excursion leading to domed appearance
- Small proportion of patients have dysplastic valve with trileaflets that are thickened and myxomatous (less commonly associated with post-stenotic dilation of MPA)
- On echo appear markedly thickened and immobile
- Important to identfiy as balloon valvuloplasty less effective
- Acquired:
- Carcinoid is most common. Other causes include rarely rheumatic heart disease, endocarditis and trauma
1 PLAX RVOT
2 PLAX RVOT Colour
PLAX RVOT CW PR
PLAX RVOT CW PS
PLAX RVOT PW Sub 1
PLAX RVOT PW Sub 2
PLAX RVOT PW Valve
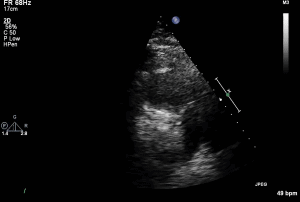
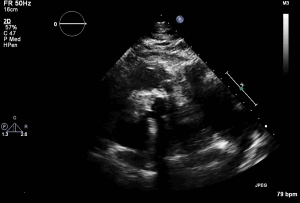
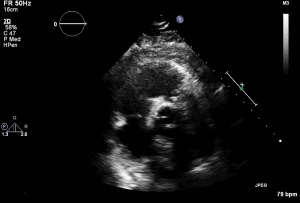
PSAX RVOT
PSAX RVOT Colour
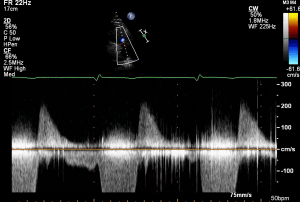
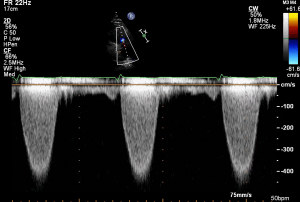
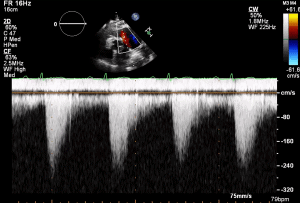
PSAX RVOT CW
A4C
RV
- History of carcinoid heart disease with previous tricuspid replacement
- Progressive pulmonary stenosis and shortness of breath
- TTE shown 1 day prior to pulmonary valve replacement
- Severe PS with max velocity 4.6m/s and mean gradient 84.6mmHg
- Moderate PR
- Mod-Severe RV dysfunction
- Carcinoid involvement of pulmonic valve classically showed thickened valve with restricted motion
Thank you Dr. Dias and Diamantouros for the case.
PLAX RVOT
PLAX RVOT Colour
PLAX RVOT CW
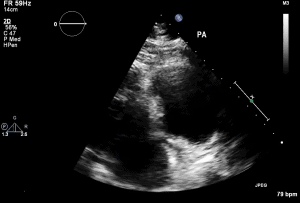
PLAX RVOT PA
PSAX RVOT
PSAX RVOT CW
- History of rheumatic heart disease with previous aortic replacement and persistent mitral stenosis
- TTE shown from 2014 but in 2020 progressed to severe and underwent pulmonic replacement
- Moderate PS with max velocity 3.1m/s and mean gradient 39.3 mmHg
- Etiology of PS thought to be congenital
- Mild PR
- Severe pulmonary artery dilation
Subvalvular
- Fibromuscular narrowing below the pulmonary valve
- Congenital
- Associated with VSD, Double Chamber RV, TOF
- Acquired
- Severe RVH (can be seen in pulmonary valvular stenosis which often resolves after intervention), prior surgery, and hypertrophic or infiltrative cardiomyopathy
- Note: Muscular infundibular obstruction is characterized by late peaking jet that appears dagger shaped (dynamic nature) which can be helpful to differentiate from fixed valvular stenosis (earlier peaking)
Supravalvular
- Discrete narrowing at MPA, bifurcation, branch vessels (can be at multiple sites)
- Congenital
- Rare but associated with different syndromes (Noonans, Williams, Rubella)
- Acquired
- Iatrogenic post-surgical repair, external compression of pulmonary artery (ie. thoracic tumour)
- Note: PV gradient should made up most of RVSP if single site of stenosis
Notes
- Right sided gradients are in series
- PA systolic pressure = RVSP – PV gradient thus PS may be mistaken for significant PH
- In severe RV dysfunction the RV cannot generate enough pressure to overcome the stenosis thus gradient can underestimate severity
- Left to right shunt or PR can increase flow across pulmonary valve and thus over estimate severity
- Doppler gradients can be less reliable in serial obstructions (ie. valvular and subvalvular/supravalvular PS)
Management
- No guideline medical management.
- If right heart failure, diuretics recommended
- Patients should follow with an Adult Congeital Heart Disease specialist
- Echocardiography should be repeated every 1-2 years depending on severity of disease and anatomic or hemodynamic sequelae
- Balloon valvulotomy preferred for valvular PS
References
- 2018 ASE: Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults
- 2018 AHA Guideline for the Management of Adults With Congenital Heart Disease
- 2017 Current Opinion in Cardiology: Imaging of the pulmonary valve in adults (html)
- 2019 BMJ: Pulmonary valve stenosis in the adult patient: pathophysiology, diagnosis and management. (html)
- 2009 ASE: Echocardiographic assessment of valve stenosis