Objectives
- Define and characterize pulmonary hypertension
- Interpret basic hemodynamics from a right heart catheterization (mean pulmonary artery pressure, pulmonary capillary wedge pressure, cardiac output, etc.)
- Differentiate between pre-capillary and post-capillary pulmonary hypertension
- Start work up for pulmonary hypertension and its causes
- Basic management for the different classes of pulmonary hypertension
Introduction
Pulmonary hypertension is a serious condition caused by multiple etiologies, characterized by elevated pulmonary artery pressure (PAP). It is associated with progressive right ventricular failure, significant morbidity, and mortality.
The hemodynamic definition was historically, a mean pulmonary artery pressure (mPAP) > 25mmg Hg, determined via right heart catheterization (RHC).
New data have shown that the normal mPAP at rest is 14+3 mmHg with an upper limit of normal of approximately 20 mmHg.
Current CCS recommendation suggest a mPAP of >20mm Hg (and PVR > 3 wood units – again by RHC) as a new cut off for defining PH.
Classification and Presentation
WHO Classes of Pulmonary Hypertension
- Pulmonary Arterial Hypertension
- Pulmonary Hypertension as a result of left heart disease
- Pulmonary Hypertension as a result of hypoxic lung disease
- Pulmonary Hypertension as a result of chronic thromboembolic pulmonary hypertension and other pulmonary artery obstructions
- Pulmonary Hypertension due to miscellaneous causes
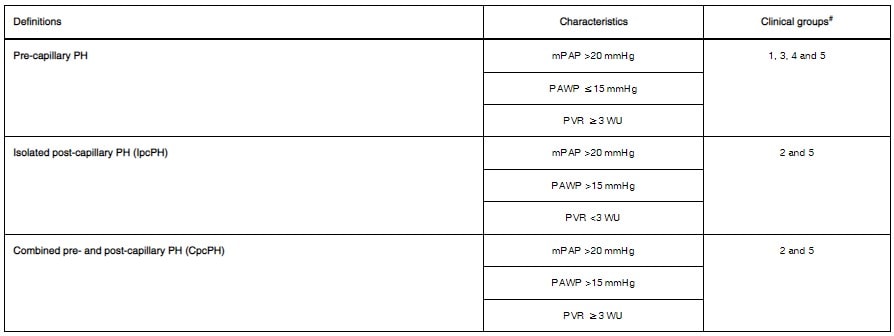
Other definitions:
- PH can be categorized by pre and post capillary with capillary being the link between the pulmonary arteries and pulmonary veins
- Pre-capillary PH: pulmonary hypertension due lungs, pulmonary artery etc (Group 1, 3, 4, 5)
- Post-capillary PH: pulmonary hypertension due to left sided heart disease (Group 2)
- Combined pre- and post-capillary PH: pulmonary hypertension due to both left sided heart disease and non-left sided heart disease determined by right heart catheterization
Workup
History
Historical features vary, it may be difficult to diagnose pulmonary hypertension (PH) given its overlap with other conditions noted above in the differential diagnosis section.However, some features of PH are:
- General:
- Asymptomatic (early on)
- Exertional dyspnea
- Palpitations
- Fatigue
- Chest pain
- Syncope (late symptom)
- Edema
- Related to mechanical complications (increase blood flow, change in bronchial artery architecture, compression of other structures – airway, nerves, etc.)
- Hemoptysis
- Voice Hoarseness
- Wheezing
Physical Exam
- Physical exam targetting the causes and complications of pulmonary hypertension
- Cardiac exam:
- Left parasternal lift
- Accentuated pulmonary component of the second heart sound (over the pulmonic area, P2),
- Third heart sound (S3)
- Pansystolic murmur of tricuspid regurgitation
- Diastolic murmur of pulmonary regurgitation
- Elevated jugular venous pressure
- Peripheral edema
- Cool extremities
- Respiratory exam:
- Velcro Crackles (Interstitial lung disease)
- Wheezing (COPD)
- Silent chest (Advanced Emphysema)
- Abdominal Exam:
- Hepatomegaly (Pulmonary HTN, also liver disease)
- Ascites (Pulmonary HTN, Liver disease)
- Telangiectasia (Scleroderma)
- Spider nevi (Liver disease)
- Testicular atrophy (Liver disease)
- Extremities:
- Telangiectasia (Scleroderma)
- Digital Ulceration (Scleroderma)
- Sclerodactyly (Scleroderma)
- Clubbing (PVOD, cyanotic CHD, interstitial lung disease or liver disease)
- Raynaud’s (Connective Tissue Disease)
- Calcinosis (Scleroderma)
Investigations
- Diagnosis of PH requires a clinical suspicion based on symptoms and physical examination and review of the investigations listed below (including the gold standard test – Right heart catheterization).
- Blood work: CBC, electrolytes, creatinine, LFTs, liver US, BNP, TSH, Thrombophilia screening (including antiphospholipid antibodies, anticardiolipin antibodies and lupus anticoagulant), HIV, Hepatitis B, Hepatitis C RF, ANA, Anti-centromere, dsDNA, anti-Ro, U3-RNP, B23, Th/To and U1-RNP
- ECG: more likely to be abnormal in advanced disease:
- P pulmonale – due to RAH
- R axis deviation
- T wave inversion in R precordial leads
- Right bundle branch block
- Atrial arrhythmias
- QT prolongation
- Rare for ventricular arrhythmias to occur
- CXR:
- Central pulmonary artery dilatation
- RA-RV dilatation
- Pruning (loss) of the peripheral blood vessels (oligemia)
- Lung disease (fibrosis, hyper-expansion in obstructive lung disease)
- Pulmonary Function Tests and Arterial Blood gas:
- Can have mild to moderate reduction of lung volumes related to disease severity.
- Low or more infrequently normal DLCO <45%predicted – poor outcomes)
- Obstructive vs Restrictive pattern
- High Resolution CT
- if needed (parenchymal lung disease, PVOD)
- Ventilation/Perfusion scan
- (Better sensitivity for CTEPH than CTPA)
- Sleep study or Overnight oximetry
- (if concern for sleep apnea)
- Cardiac MR in cases
- where echo is inconclusive
- Prognostication
- 6-minute walk test
- Cardiopulmonary test / VO2 max
Transthoracic Echocardiogram
- First line test for patients suspected of PH to estimate pulmonary artery pressure, assess for potential cause (left heart disease) and look for consequences (RV dilation/dysfunction)
- Not sufficient for definitive diagnosis – but can identify features suggestive of PH (gold standard is right heart catheterization)
- Can be helpful in determining a cause (e.g. left sided pathology as a cause of PH)
- Important tool in follow up (increase in PAPs does not usually reflect disease progression). Important factors include:
- Chamber sizes (RA, RV area)
- Magnitude of TR
- LV eccentricity index
- RV contractility (determined by RV longitudinal systolic strain and RV fractional area change, Tei Index and tricuspid annular plane of systolic excursion -TAPSE)
- Presence of pericardial effusion
Right Heart Catheterization
- Gold standard procedure for diagnosis of pulmonary hypertension
- Technical considerations in performing RHC
- Appropriate positioning of pressure transducer at midchest height.
- Measurement of wedge pressure at end expiration.
- Ideally this procedure should be performed at an expert center before proceeding with treatment (particularly in PAH, CTEPH, etc.). Important parameters are highlighted below:
- Look for a shunt (oximetry run)
- Wedge pressure – surrogate for left atrial pressure (end of expiration, to reduce impact of intrathoracic pressure)
- Left ventricular end-diastolic pressure (LVEDP): may need 500 mL bolus PRN to reveal diastolic dysfunction
- Cardiac output: Thermodilution (in the absence of significant TR or low output state or shunt) or Fick
- PVR (WU) = (mPAP – Wedge) / Cardiac output
- Diastolic pressure gradient = dPAP – Mean Wedge (helpful for determining pre and post capillary or mixed/combined pulmonary hypertension)
- Vasoreactivity testing for identification of patients suitable for high-dose calcium channel blocker (CCB) treatment is recommended only for patients with Idiopathic PAH, Heritable PAH or drug-induced PAH; done with epoprostenol or adenosine IV or inhaled nitric oxide
- Positive: absolute decrease of mPAP ≥ 10 mmHg (to mPAP < 40 mmHg) in the absence of decreased cardiac output
- Hepatic venous pressure gradient = Wedged hepatic venous pressure – IVC pressure;
- Normal value between 1-5 mmHg (≥ 10 mmHg A portal hypertension / cirrhosis)
Management
- Depends on the underlying etiology and subsequent management of said etiology. However, there are general guidelines in management of these patients.
- General Recommendations:
- PAH patients should avoid pregnancy
- Immunize against pneumococcal infection and influenza
- Enrolling in a physical rehabilitation program
- Oxygen in those that qualify (aim for PaO2 > 60mmgHg, SPO2 > 90%)
- Psycho-social Support
- Refer to PH expert care
Group I Pulmonary Hypertension
- PAH must be diagnosed by excluding other more common etiologies (left heart disease, lung disease, and CTEPH)
- Vasoreactivity testing in select PAH patients as mentioned above
- Risk stratification using a combination of clinical, hemodynamic, and imaging features
Medical Therapy for PAH:
- Broad goal is to reduce the pressure in the pulmonary artery vasculature
- Management is initiated with oral vs intravenous and mono vs dual therapy depending on risk and stability of patient
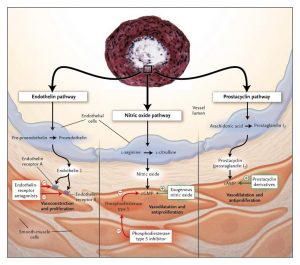
- PH medications work by different pathways (endothlin, nitric oxide, and prostacyclin) and classes include calcium channel blocker, prostacyclines, endothelin antagonists and PDE5 inhibitors
- Calcium Chanel Blockers (Idiopathic PAH, Heritable PAH or drug-induced, with vasodilator response)
- Nifedipine
- Amlodipine
- Diltiazem
- Prostacyclines analogues/Prostanoids
- Beraprost
- Epoprostenol
- Iloprost
- Treprostinil
- Prostacyclin IP agonist
- Selexipag
- Endothelin Antagonists
- Bosentan
- Maticentan
- Ambrisentan
- Phosphodiesterase-5 Inhibitors and Guanylate Cyclase simulators
- Sildenafil (PDE5 inhibitor)
- Tadalafil (PDE5 inhibitor)
- Vardenafil (PDE5 inhibitor)
- Rociguat (sGC simulator)
- Calcium Chanel Blockers (Idiopathic PAH, Heritable PAH or drug-induced, with vasodilator response)
Angicoagulation in PAH:
- CCS suggests systemic anticoagulation with warfarin in selected PAH patients (idiopathic PAH, heritable PAH, drug- and toxin-induced) in the absence of elevated bleeding risk. (Although this is based on weak evidence based on observational data showing in situ thrombosis of patients with PAH)
Follow-up:
- Patients should be reassessed in 3-4 months time post institution or change in therapy
- If deemed low risk follow up can be done in 6-12 months time
Group II Pulmonary Hypertension
- Initial management is to manage the underlying condition (Systolic Failure, Diastolic Failure, Valvular disease, etc.) and institute aggressive diuresis to maintain euvolemia
- Manage underlying risk factor for cardiac disease (Metabolic syndrome, Diabetes)
- Rule out and manage other contributing causes: Sleep apnea, COPD
- May consider device therapy in advanced heart failure, with pulmonary hypertension
Group III Pulmonary Hypertension
- Currently there is no specific therapy for PH associated with lung diseases.
- Rule out other contributing causes of PH
- Long-term O2 administration has been shown to partially reduce the progression of PH in COPD
- Treat the underlying lung disease (COPD, ILD, Sleep Disorders, etc.)
- No good evidence for PAH drugs
- Lung Transplant
Group IV Pulmonary Hypertension
- Consider the differential diagnosis of CTEPH.
- These conditions include PA sarcoma, tumour cell embolism, parasites (hydatid cyst), foreign body embolism and congenital or acquired PA stenosis.
- Screening
- CCS recommends that patients with residual dyspnea or exercise intolerance after at least 3 months of uninterrupted anticoagulation post acute PE be assessed for CTEPH with echocardiography and V/Q lung scan.
- Medical treatment:
- Anticoagulation (for life)
- Off label use of PH medications (if not surgical candidate)
- Riociguat (some evidence for it in recurrent CTEPH, or non surgical candidates)
- Surgical treatment:
- Gold standard is pulmonary artery endarterectomy done at an expert center
- Consider balloon pulmonary angioplasty if non operable
- Lung transplant
Group V Pulmonary Hypertension
- Treat underlying cause of the pulmonary hypertension
- No other therapies/vasodilators have been proven effective
Further Reading
- 2020 Canadian Cardiovascular Society/Canadian Thoracic Society Position Statement on Pulmonary Hypertension (html) (pdf)
- 2019 Proceedings of the 6th World Symposium on Pulmonary Hypertension (html)
- 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension (html) (pdf)
- Diagnosis of chronic thromboembolic pulmonary hypertension: A Canadian Thoracic Society clinical practice guideline update (pdf)
- Cardiology: A practical handbook by David Laflamme
Authors
- Primary Author: Dr. Dimitar Saveski (MD, FRCPC, Internal Medicine Resident)
- Author/Reviewer: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Staff Reviewer: pending (MD, FRCPC[Cardiology])
- Last Updated: June 3, 2021
- Comments or questions please email feedback@cardioguide.ca