Abbreviations
- MACE – Major Adverse Cardiac Effects (mortality, infarction, cardiovascular death, etc)
- UA – Unstable Angina
- NSTEMI – Non-ST Elevation MI
- cTn – Cardiac Troponin
- NPV – Negative Predictive Value
Diagnosis
History
Helpful Features:
- Prior MI
- Risk factors (age, gender, hx of CAD)
- Deep, poorly localized, chest/arm pain
- Worse with exertion / emotional stress
Features NOT Helpful (studied)
- Relieved with nitro
(35% with ACS, 41% without ACS) - Relieved with GI antacids like “pink lady”
Features not characteristic
- Pleuritic 13%
- Sharp or knife-lung in respiration (22%)
- Midline or lower abdomen
- Pain localized with 1 finger
- Pain reproduced with arm movement or palpation (7%) (high NPV)
- Brief episodes (few seconds or less)
- Maximal at onset
NOTE: Historic characteristics increase/decrease likelihood that chest pain is ischemic, but none rule it out
Diagnostic Tests
- 12-lead ECG (Repeat if diagnosis is unclear) – at 15-30min intervals if high risk of suspicion
- NSTEMI ECG could have persistent or transient ST depression, transient ST elevation, T-wave inversion, flat T waves, pseudo-normalization of T waves or it can be normal.
Cardiac Biomarkers
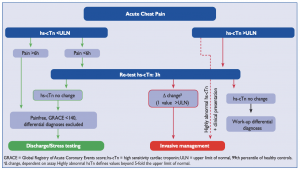
- Serial cardiac Troponin I or T at presentation and at 3-6hrs after SYMPTOM onset (AHA 2014)
(ESC 2015 promotes 0/3hr from PRESENTATION; 0/1hr algorithms validated for some assays)- Additional troponin level can be obtained beyond 6 hours in patients with normal serial troponin levels if there is intermediate/high suspicion for ACS
- High-sensitivity cTn rises within 1h, and can remain elevated for days/weeks.
- Repeating troponin levels until they “peak” is not recommended and is not helpful. Checking the troponin more than 3 times is generally a poor use of resources.
- However, additional biomarker measurement on day 3 or 4 can help prognosticate and determine infarct size (particularly CK)
- NOTE: If your institution has Troponin T, assume it is “high-sensitivity.” Troponin I has many assays, but most modern institutions use high-sensitivity Troponin I assays.
- CK-MB
- Released from myocardium much more rapidly, and “peaks” earlier than troponin.
- Generally less sensitive than troponin, and less specific for myocardium
- May correlate better to infarct size
- May be helpful if you suspect patient is having a second ACS event, and troponin is still rising from the initial event
- Serial cardiac Troponin I or T at presentation and at 3-6hrs after SYMPTOM onset (AHA 2014)
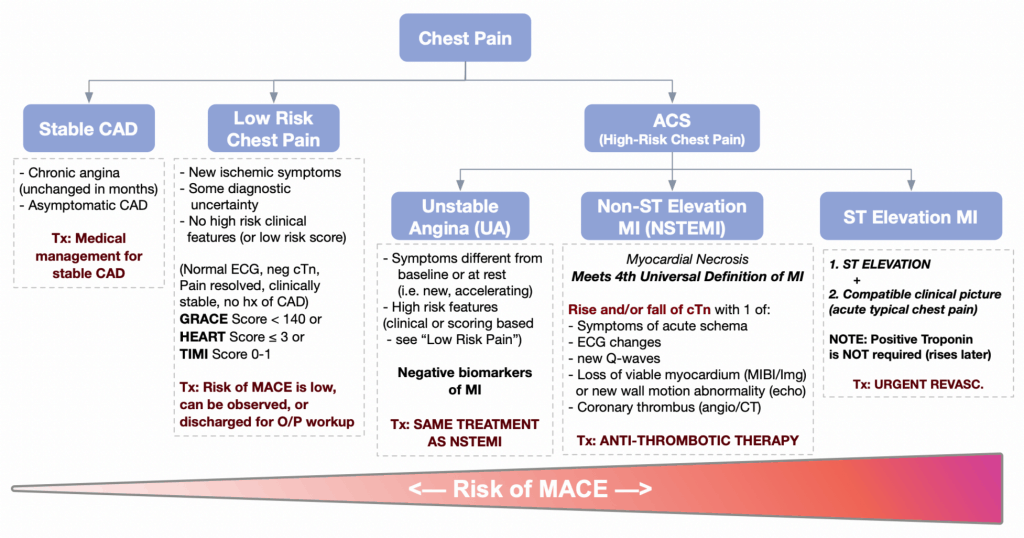
Approach to Chest Pain & Classification
- Initial assessment of patients should:
- Establish likelihood that chest pain is due to myocardial ischemia
- Rule out other main causes of chest pain (aortic dissection, PE, pericarditis)
- Classify patients into the following categories:
- STEMI, NSTEMI, unstable angina, low risk chest pain, and stable angina (see below)
- Risk stratify the patient into “high risk of MACE” or “low risk of MACE” clinically
- (NOTE: Does not apply to STEMI, which is always considered high risk)
- Categories of patients presenting with ischemic chest pain:
- STEMI – ST elevations with compatible clinical picture
- NSTEMI – Rise and fall of cardiac biomarkers, which meets the Universal Definition of MI
- Unstable Angina – New/rest/changing pain without cTn or ECG changes, but “High Risk of MACE” (see below)
- Generally benefit from admission and aggressive antithrombotic therapy; so treated the same as NSTEMI
- Low Risk Chest Pain – New/rest/changing pain without cTn or ECG changes, but “Low Risk of MACE” (see below)
- Generally benefit less from aggressive/invasive therapy. These patients can be treated with observation/outpatient management with ASA, nitro spray, activity precautions until further assessment is done
- Stable Angina – Predictable retrosternal chest pressure worse on exertion/stress, better with rest/nitroglycerin. To be “stable,” the pain must remain unchanged for at least 2 months.
- NOTE: Patients with stable angina who have a change in the pain, such as worsening pain, brought on by less exertion, or pain at rest, should be risk stratified to unstable angina or low risk chest pain.
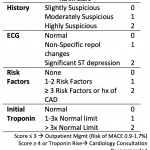
- How do I know if my patient is “Low Risk of MACE” or “High Risk of MACE”? You must risk stratify them using one or more of the tools below:
-
- Clinical picture (Normal ECG? resolution of chest pain? history of CAD? clinically stable?)
- HEART Score ≤ 3 (New, well-validated, best correlates to 30d risk of MACE)
- GRACE Score < 140 (Endorsed by ESC Guidelines 2015, better c-statistic than TIMI score)
- TIMI Score 0-1 (Endorsed by AHA Guidelines 2014)
- Stress Test (if able to obtain quickly)
-
- NOTE: You should know the main categories of the HEART and GRACE scores to quickly risk stratify ACS patients clinically.
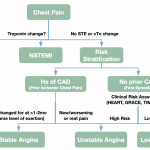
Low Risk Chest Pain
- No ST elevation + no cTn change + and deemed low risk through:
- Clinical assessment OR
- Scoring tools (i.e. HEART, GRACE, TIMI) – see “Approach” section above
- There is often diagnostic uncertainty as to the cause of chest pain
- Risk of MACE is low, and after a period of observation (+/- 3rd cTn) these patients can often be managed in an outpatient setting with close follow-up:
- ASA is recommended (Class IIB)
- Risk factor modification
- These patients benefit less from intensive anti-thrombotic therapy and revascularization.
- Those who may benefit may be further selected with non-invasive risk stratification:
- Treadmill Stress ECG (functional test)
- Myocardial Perfusion Imaging (MIBI) (functional test)
- Stress Echocardiography (functional test)
- Coronary CT (anatomic test – can exclude ACS/CAD)
- Those who may benefit may be further selected with non-invasive risk stratification:
Unstable Angina
- Generally considered to be an ACS (plaque rupture/instability), but amount or duration of ischemia is insufficient to cause myocardial infarction and elevate biomarkers.
- Classic patient is someone with on/off chest pain that lasts <30-60min at a time.
- To call UA, there should NOT be any rise/fall of cTn on serial testing, and there should be concern that the chest pain is “high risk” based on clinical assessment or scoring (HEART, GRACE or TIMI)
Management
- Hospital admission with medical management is the SAME as NSTEMI to treat plaque rupture/instability (see below)
- Compared with NSTEMI, there is less benefit with revascularization
- Patients can be selected for further risk stratification to determine if they will benefit from revascularization through non-invasive tests (i.e. exercise ECG, stress echo, MIBI, Cardiac CT
- Based on numerous factors, some clinicians may prefer invasive coronary angiography
Practical Tip: New studies indicate that in the modern era of high-sensitivity cTn, negative cTn is excellent at predicting low risk of MACE. Overall the diagnosis rate of UA is declining. Most of the cTn-negative patients are classified as “Low Risk Chest Pain.”
NSTEMI
- Must qualify as “Myocardial Infarction (MI)”, which is based on the Universal Definition of MI
- Patients with NSTEMI should generally be admitted to hospital and treated with antithrombotic therapy (below)
| 4TH UNIVERSAL DEFINITION OF MI |
|---|
Rise and/or fall of cTn with 1 of:
|
Management: Symptom Management
- Oxygen: Supplemental only if sat ≤ 90% (routine O2 = poor outcomes)
- Nitrates:
- Indications: Chest pain, HF, hypertension
- Benefit: Symptoms only (no effect on MACE)
- Doses/Options: Nitro spray 0.4mg q5min x3
- If pain beyond 3 nitro sprays, start infusion
- Infusion Dose: 20 mcg/min IV → increase by 20 mcg/min increments until pain is controlled (max 400 mcg/min)
- If infusion is not desired or the patient has intermittent chest pain, a nitro patch can be considered (or a low dose infusion): 1.2 mg/hr patch is equivalent to 20 mcg/min infusion
- Contraindications:
- PDE Inhibitors: within 24 hours of sildenafil or vardenafil, or within 48 hours of tadalafil
- Hypotension
- NOTE: Chest pain refractory to antithrombotic therapy and nitrates is an indication for immediate invasive therapy.
- Morphine:
- Indications: Only if pain refractory to all anti-ischemic agents
- Suggestion of harm – (i.e. interference with anti-platelet agents, risk of HF, etc.)
Management: Antithrombotic Therapy
- Dual Antiplatelet Therapy
- Indications: All post-MI patients
- Benefit: CV mortality, recurrent MI, need for revasc, etc. (MACE)
- PLATO (ticagrelor), CURE (clopidogrel), TRITON-TIMI38 (prasugrel)
- Duration > 1yr: PEGASUS-TIMI 54
- Doses/Options:
- ASA 160mg chew + 80mg OD thereafter indefinitely
AND one of: - 1st Line: Ticagrelor 180mg + 90mg BID thereafter (at 1y change to 60mg bid for up to 3y total)
- 1st Line: Prasugrel (Also considered first-line option, but no longer available in Canada)
- 2nd Line: Clopidogrel 300mg + 75mg OD thereafter (consider 160mg daily x6d post-PCI)
Continue 75mg for up to 3y post-MI (CCS 2018)
- ASA 160mg chew + 80mg OD thereafter indefinitely
- Switching: Switching between ticagrelor and clopidogrel → always reload (CCS 2018)
- Contraindications:
- Prasugrel contraindicated if prior TIA/Stroke (not available in canada)
- Ticagrelor contraindicated if previous intracranial hemorrhage
- No ticagrelor load if > 75 yo (AHA 2014)
- Add PPI if has risk factors for GI bleed (prior bleed, etc.)
- Anticoagulation
- Indication: ALL post-MI patients
- Options/Doses:
- 1st Line: Fondaparinux 2.5 mg SC daily
- OASIS-5 Trial: Less bleeding than enoxaparin, higher risk of catheter thrombosis (requires heparin load in cath lab)
- Continue for 8 days, until PCI, or until discharge; usually continue through hospitalization as DVT prophylaxis
- 1st Line: Unfractionated heparin 60 IU/kg (max 4000 IU) infuse 12 IU/kg (max 1000 IU/kg), target aPTT
- Old studies, pre-DAPT era
- Stop at revascularization, discharge or 48hrs (whichever comes first)
- 1st Line: Enoxaparin 1mg/kg SC q12h (OD dosing if CrCl < 30 mL/min)
- Patients for non-invasive approach: ESSENCE Trial: superior to heparin for mortality (continue through hospitalization or until PCI performed).
- Patients for invasive approach: Many interventional cardiologists recommend against enoxaparin if patient is undergoing invasive approach (SYNERGY Trial: comparable to UFH in efficacy in pts undergoing invasive approach, but increased risk bleeding)
- 2nd Line: Bivalirudin (expensive in Canada, generally used in patients with HIT)
- 1st Line: Fondaparinux 2.5 mg SC daily
- PRACTICAL TIP:
- If PCI is planned, guidelines recommend any of the three first line agents but UFH is often preferred. In modern studies, enoxaparin showed similar outcomes but increased in-hospital major bleeding (SYNERGY) and fondaparinux had increased catheter thrombosis during angiography requiring a bolus of heparin (OASIS-5). OASIS-5 results also suggest that patients at high risk of bleeding can be considered for fondaparinux.
- If conservative/medical management is planned guidelines prefer fondaparinux or enoxaparin over heparin due to improved outcomes/convenience and decreased bleeding (ESSENCE). Again, in patients at high risk of bleeding, fondaparinux is preferred (OASIS-5)
- GPIIB/IIIA inhibitors – Only used by interventional cardiology for bailout situations / thrombotic complications.
Management: Adjunctive Therapies
Management: Revascularization
Guidelines
Unlike STEMI, the benefit of revascularization of UA/NSTEMI without “high-risk features” has been controversial. (See “Evidence for revascularization strategies” below.)
Physicians should select an approach based on risks/benefits, and patient/physician preference.
Available Approaches
- Routine Invasive: Invasive diagnostic evaluation (angiogram) +/- PCI for ALL patients
- Early Invasive Strategy -> within 24hrs
- Delayed Invasive Strategy -> within 25-72hrs
- Ischemia Guided Strategy: Medical management. Invasive intervention only if:
- Failure of medical therapy (ongoing ischemic chest pain)
- High prognostic risk (TIMI/GRACE)
- High-risk non-invasive stress test
- If reasonable, a non-invasive risk stratification test can be used to determine if the patient is “high/intermediate risk” and may benefit from invasive management (most commonly MIBI)
| AHA 2014 & ESC 2015 (see strategies to the right) |
| Indications for Invasive Evaluation in UA/NSTEMI |
|---|
Urgent / Immediate Invasive Strategy
Early Invasive Strategy (within 24hrs)
Ischemia Guided Strategy (Conservative)
(Review the ESC and AHA algorithms to the right) |
Summary of Evidence
- FRISC-II Trial (1999) – Intermediate to high risk patients (FRISC score)
- Early invasive strategy >> Ischemia-Guided (fewer recurrent MI and improved long-term survival)
- Very old trial – poor medical therapy available at that time.
- Definition of MI had issues (i.e. Troponin often not used, peri-procedural MI missed)
- TACTICS-TIMI 18 Trial (2001) – pts with unstable angina and NSTEMI
- Early Invasive >> Medical Management (only if TIMI > 2)
- ICTUS Trial (2005) – Pts with elevated troponin.
- Early invasive = Ischemia Guided
- Most recent data with relatively modern medical therapy.
- RITA-3 Trial (2002) – pts with non-ST-elevation ACS
- Early Invasive >> Medical Management for “refractory angina”, equal for death and MI
- Meta-Analysis of 7 RCTs: (Bavry JACC 2006)
- Early Invasive >> Med Mgmt for NSTEMI
Bottom Line:
- Revascularization appears to consistently confer a benefit in reducing angina, and possibly mortality benefit ONLY in “high/intermediate risk” groups.
- Overall, trials controversial due to non-standard risk-stratification methods and variable definitions of MI.
- ESC 2015 guidelines recommend routine invasive management if there is a troponin change
- AHA 2014 guidelines recommend either approach, leaning towards early invasive in patients with high or intermediate risk. (To estimate risk, use GRACE, TIMI, or table above)
References
Highly-Recommended Reading
- AHA/ACC 2014 – Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes
- ESC 2015 – Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
- CCS 2018 (Antiplatelet Therapy Update) – Focused Update of the Guidelines for the use of Antiplatelet Therapy
- CCS 2012 (Antiplatelet Therapy) – Antiplatelet Therapy Guidelines 2012 Update: The Use of Antiplatelet Therapy
Optional Reading
- Primary Author: Dr. Pavel Antiperovitch (MD, FRCPC, Cardiology Fellow)
- Author/Reviewer: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Staff Reviewer: Dr. Terrance McPherson (MD, FRCPC[Cardiology])
- Copy Editor: Perri Deacon (medical student)
- Last Updated: Feb 26, 2022