Abbreviations
- MS: mitral stenosis
- MR: mitral regurgitation
- AF: atrial fibrillation
- CCS: Canadian Cardiovascular Society
- ACC: American College of Cardiology
- AHA: American Heart Association
Background
Causes
- Majority of cases worldwide are due to rheumatic heart disease (most commonly affects the mitral valve)
- In high-income countries calcific mitral stenosis is increasingly more common
Hemodynamics
- Patients with mitral stenosis have an obstruction of flow from the left atrium to the left ventricle.
- This generates high atrial pressures, which can cause pulmonary edema, pulmonary hypertension, and eventually right sided heart failure.
- The natural history of MS is “disease of plateaus”. Patients generally do well, but have periods where their symptoms are worse.
- NOTE: Unlike aortic stenosis, aortic regurgitation, and mitral regurgitation, clinicians can wait before intervening on severe MS since waiting does not have any permanent hemodynamic effects on the LV.
History & Physical
History
- Patients generally present with shortness of breath on exertion and decreased exercise tolerance
- Less commonly they may have hemoptysis (elevated pulmonary pressure), palpitations (atrial fibrillation), fatigue, or stroke (thromboembolism from atrial fibrillation)
Physical exam
- Cardiac exam:
- Palpation: RV heave may be present with pulmonary hypertension
- Heart Sounds: loud S1 that becomes softer as stenosis becomes worse, loud P2 (pulmonary hypertension), and progressively single S2
- Opening snap heard at the apex after S2
- Diastolic murmur best heard at the apex
- Volume: crackles may be present if there is pulmonary edema and in advanced disease, right heart failure may be present
Investigations
ECG: Most important feature to assess for is presence of atrial fibrillation. Left atrial enlargement (p wave >0.12s in lead II) or p-mitrale may be present. P-mitrale is a bifid P-wave (M-shaped) in Lead II suggesting left atrial enlargement in mitral stenosis.
Chest X-Ray: Assess for heart failure and evidence of left atrial enlargement
Echocardiography:
Transthoracic echocardiography is used to confirm severity of mitral stenosis and determine etiology (i.e. rheumatic vs non-rheumatic).
It can also look for consequences such as left atrial enlargement, pulmonary hypertension, and right ventricular size/function. The left ventricle is usually unaffected.
Echocardiography (TTE +/- TEE) is important to assess for suitability for balloon commissurotomy if rheumatic mitral stenosis.
Mangement
Asymptomatic MS
- In asymptomatic MS, serial monitoring with echocardiograms is indicated. Timing of follow-up interval is based on severity of MS.
- Generally safe to wait until symptoms arise (unlike other valvular abnormalities, where symptoms indicate end-stage disease).
Stroke Prevention
- Prevention of thromboembolism is very important as high rate of atrial fibrillation
- If patient has severe MS, anticoagulation is recommended if:
- Atrial fibrillation
- History of embolism (even without atrial fibrillation)
- Left atrial thrombus
- Warfarin is first line for patients with moderate-severe mitral stenosis (rheumatic or non-rheumatic) as per CCS 2020 Atrial Fibrillation guidelines
Symptomatic severe MS
Medical Management
- Heart failure management with diuretics as needed
- Patients with severe MS do not tolerate tachycardia (sinus or AF) given reliance on diastolic filling time for preload, thus heart rate control is important
Valve Intervention
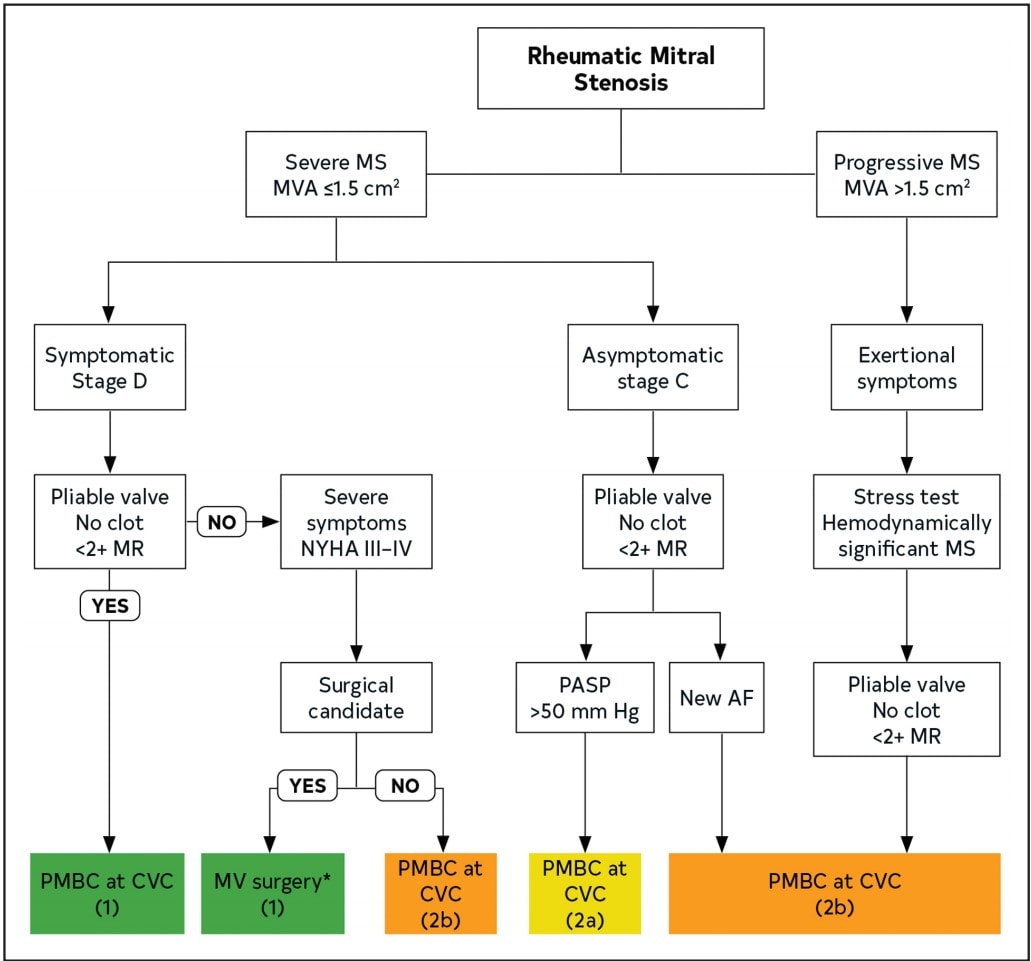
- Rheumatic Mitral Stenosis Indications for Intervention
- Severe MS + symptoms (Class 1)
- Severe MS + pulmonary hypertension or new AF (Class 2)
- Percutaneous balloon valvotomy is preferred if valve anatomy is favourable (less than moderate MR)
- Otherwise should go for mitral valve surgery
- Non-rheumatic Calcific Mitral Stenosis
- No Class 1 indication for surgery
- If severe MS and severely symptomatic, should have a risk benefit discussion with patients
- Patients with calcific MS are often older and have multiple co-morbidities, thus are generally higher risk for surgery
Authors
- Primary Author: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Reviewer: Dr. Pavel Antiperovitch (MD, FRCPC Cardiologist)
- Copy Editor: Megha Shetty (MD Candidate)
- Last Updated: Dec. 19, 2021
- Comments or questions please email feedback@cardioguide.ca