Abbreviations
- HF – Heart failure
- ARNi – Angiotensin receptor-neprilysin inhibitor
- MRA – Mineralocorticoid receptor antagonist (e.g. spironolactone and eplerenone)
- AHF – Acute exacerbation of heart failure
Definitions
| Term | Acronym | Definition |
|---|---|---|
| Heart Failure with preserved ejection fraction (HFpEF) | HFpEF | Clinical HF with LVEF ≥ 50% |
| Heart Failure with mid-range ejection fraction (HFmEF) | HFmEF | Clinical HF with LVEF 41-49% |
| Heart Failure with reduced ejection fraction | HFrEF | Clinical HF with LVEF ≤ 40% |
| Heart Failure with recovered ejection fraction | HF Recovered EF | LVEF Recovered to ≥ 40% with treatment |
Diagnosis
- Heart failure is a clinical syndrome resulting from structural and functional impairment of ventricular filling and/or cardiac output.
- During acute phase, treatment focuses on decongestion (discussed in the Acute Heart Failure topic)
- There is no single parameter or test that can diagnose heart failure, rather it is a constellation of signs, symptoms and investigations to make a diagnosis
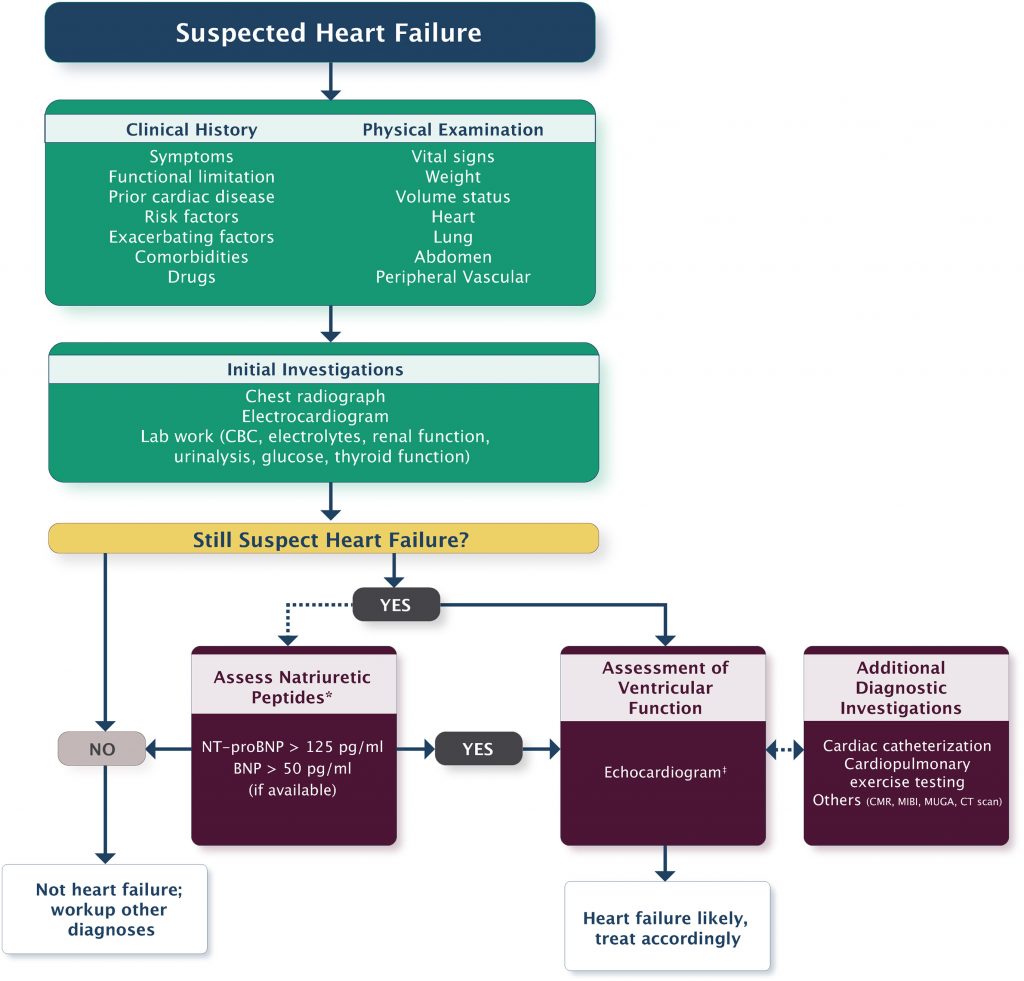
- See CCS algorithm as initial approach to a patient with suspected heart failure
Risk Factors
| Demographic | Medical History | Markers |
| Older age | Hypertension | Abnormal ECG |
| Male | CAD | Widened cardiac silhouette on CXR |
| Heavy alcohol use | Diabetes | Elevated neurohormonal biomarkers |
| Smoking | Hyperlipidemia | Elevated resting heart rate |
| Physical inactivity | Obesity | Microalbuminuria |
Symptoms
- Progressive shortness of breath (LR+ 1.3)
- Orthopnea (LR+ 2.2)
- Paroxysmal nocturnal dsypnea (LR+ 2.6)
- Ankle swelling
- Abdominal fullness
- Weight gain (LR+ 1.0)
- Nausea and/or anorexia (hepatic congestion)
- Fatigue/lethargy (LR+ 1.0)
Signs
- Elevated JVP (LR+ 5.1)
- Positive hepatojugular reflux (10s pressure, 3cm rise) (LR+ 6.4)
- Pulmonary rales/crackles (LR+ 2.8)
- Decreased air entry to bases (pleural effusion)
- S3 (LR+ 11)
- Laterally displaced apex beat
Note: JAMA Positive LR included. Full article here
New York Heart Association (NYHA) Functional Classification
| Class | Definition | Other descriptor |
|---|---|---|
| I | No symptoms | Asymptomatic |
| II | Symptoms with ordinary activities | Mild symptoms |
| III | Symptoms with less than ordinary activities | Moderate symptoms |
| IV | Symptoms at rest or with any minimal activity | Severe symptoms |
Investigations
- ECG
- Laboratory:
- CBC, Creatinine, Ferritin, TSH
- Troponin (prognostic stratification)
- BNP/NT-proBNP (if available)
- CCS: Helpful to rule in/out HF when cause of dyspnea is in doubt
- Echocardiogram
- Used to determine etiology and Ejection Fraction (most important prognostic markers and guides management)
If clinical suspicion:
- Coronary studies (coronary CT, angiogram)
- Cardiac MRI
- PET (for certain etiologies)
Etiology
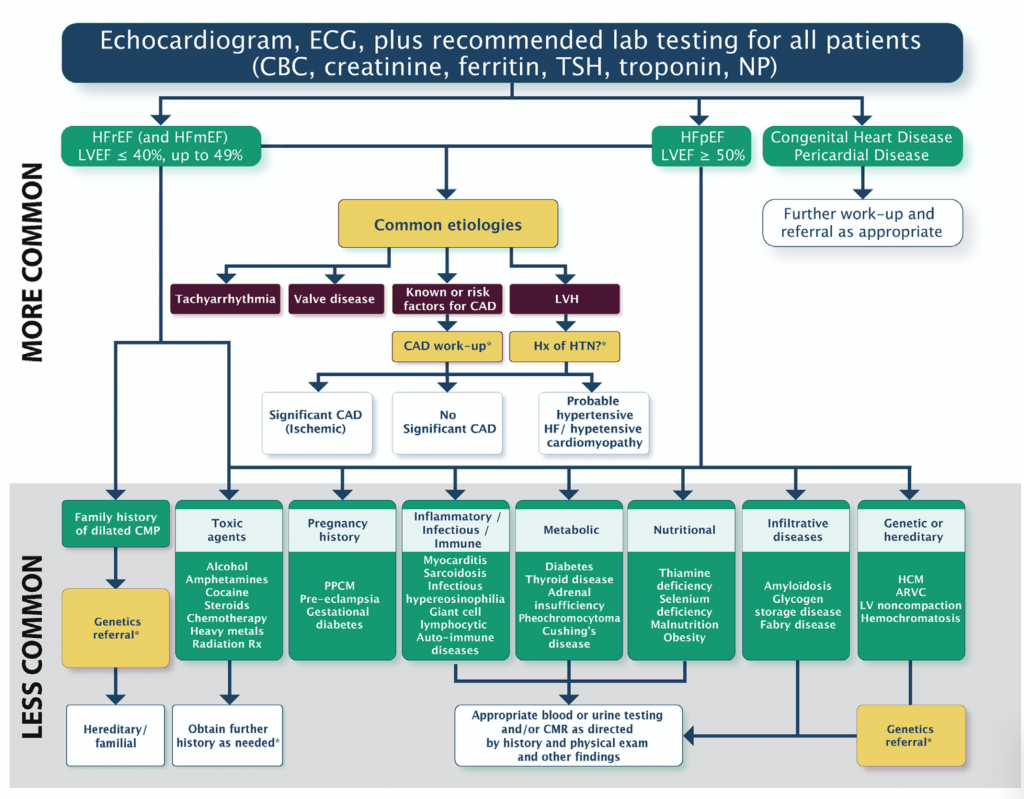
- The most common cause for HF in industrialized countries is coronary artery disease, accounting for 60-75% of all cases.
- After initial workup and ruling out common etiologies (tachyarrhythmias, valve disease, coronary artery disease, and left ventricular hypertrophy), further investigations should be tailored to patients history
- CCS algorithm (above) provides a basic framework to the different cardiomyopathies and Table 6-8 in the guideline have more information. Further details are beyond the scope of this topic and often involve expert Cardiology consultation
Prognosis
- Several models exist to convey risk to patients about the predicted mortality after developing heart failure. Here are some examples:
- Seattle Heart Failure Model: Mortality risk at 1, 2, and 5 years with or without intervention; mean life expectancy
- MAGGIC risk score: Mortality risk at 1 and 3 years
- EHMRG: 7- day mortality on presented to emergency department
Treatment (HFrEF)
Introduction to Treatment
- Guideline-directed medical treatment (GDMT) is the most important factor in improving outcomes in patients with chronic heart failure and should be initiated in all patients with HFrEF (mortality and morbidity).
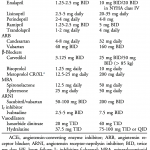
- Therapies must be up-titrated to target doses – these are the doses at which their benefit is proven (see Table).
- If target dose cannot be reached due to side-effects (such as renal failure, hypotension), can maintain on highest tolerated dose.
- Therapies are introduced in a stepwise fashion – starting with B-blocker, ACE inhibitor, and MRA.
- Once triple therapy is optimized, additional therapy such as ARNI, SGLT-2 inhibitor, ivabradine, hydralazine/isosorbide dinitrate should be added.
- Avoid stopping in routine acute illness (e.g. pneumonia, COPD exacerbation) unless not tolerated (reactive airways or hemodynamic instability).
- If stopped, reinitiate whenever possible (remember: these are life-saving medications)
- Identify patients with “advanced heart failure,” because they require special treatment considerations (see below).
- Please use the tables below as a guide.
Beta Blockers
- Alpha-1 and Beta-1 (and Beta-2) receptor antagonists
- Benefits: Reverse LV remodelling, improve symptoms, prevent hospitalizations, improve mortality
- Cautions:
- Do not start if the patient is unstable or in heart failure (negative inotropes)
- If patient presents with AHF, continue b-blocker (unless hemodynamically unstable or in shock)
- Up-titrate slowly (q2-4 weeks). Rapid uptitration can exacerbate HF.
| CCS 2017 Heart Failure Guidelines |
| Indications for Beta Blockers |
|---|
|
- Metoprolol: (MERIT-HF)
- NOTE: Trials used long-acting “succinate” formulation. Canada does not have succinate, and instead have the short-acting “tartrate” formulation, which is given twice daily.
- Start 12.5mg BID, titrate to 100mg BID
- Bisoprolol: (CIBIS-II)
- Start 1.25 – 2.5mg daily, titrate to 10mg daily
- The most selective and long-acting beta blocker; best choice in patients with obstructive lung disease
- Carvedilol: (COPERNICUS)
- Start 3.125mg BID, titrate to 25mb BID (or 50mb BID if > 85kg)
- NOTE: Carvedilol is a non-selective beta-blocker; caution in patients with hypotension and reactive airway disease
ACE Inhibitors
- Work via 2 pathways: inhibition of angiotensin II, and upregulation of bradykinin
- Benefits: Reverse LV remodelling, prevent
shospitalizations, improvessymptoms, reduce mortality - Side Effects/Cautions:
- Cough (bradykinin-mediated) in 10-20%
- If tolerable, continue
- If intolerable, switch to ARB
- Angioedema (< 1%): switch to ARB
- Hypotension, hyperkalemia
- Acute kidney injury (creatinine rise up to 30% is expected after initiation of an ACEi/ARB, do not discontinue)
- Cough (bradykinin-mediated) in 10-20%
| CCS 2017 Heart Failure Guidelines |
| Indications for ACE Inhibitors |
|---|
|
- Notable trials:
- HOPE (Risk factors of HF)
- SOLVD – Post MI, HF, EF ≤ 35%
- SAVE – Post MI, asymptomatic EF ≤ 40%
- Generally a class effect, but preferred ACE inhibitors that are proven in trials:
- Enalapril/captopril have shortest half-lives (dosed BID)
- Enalapril start 2.5mg BID, target 10-20 BID
- Ramipril is intermediate (usually BID)
- Start 2.5mg BID, target 5mg BID
- Perindopril is long-acting (daily dosing)
- Start 2mg daily, target 4-8mg daily
- Enalapril/captopril have shortest half-lives (dosed BID)
Mineralocorticoid Receptor Antagonists (MRAs)
- Work via 2 pathways: Inhibit the exchange of Na+ and K+ in the kidney causing minimal diuretic effect and aldosterone antagonism
- Benefits: Reverse LV remodelling, prevent hospitalizations, improve symptoms, reduce mortality.
- Side Effects/Cautions:
- Hyperkalemia (especially during AKI)
- Gynecomastia (with spironolactone)
| CCS 2017 Heart Failure Guidelines |
| Indications for MRAs |
|---|
|
Other Medical Therapy
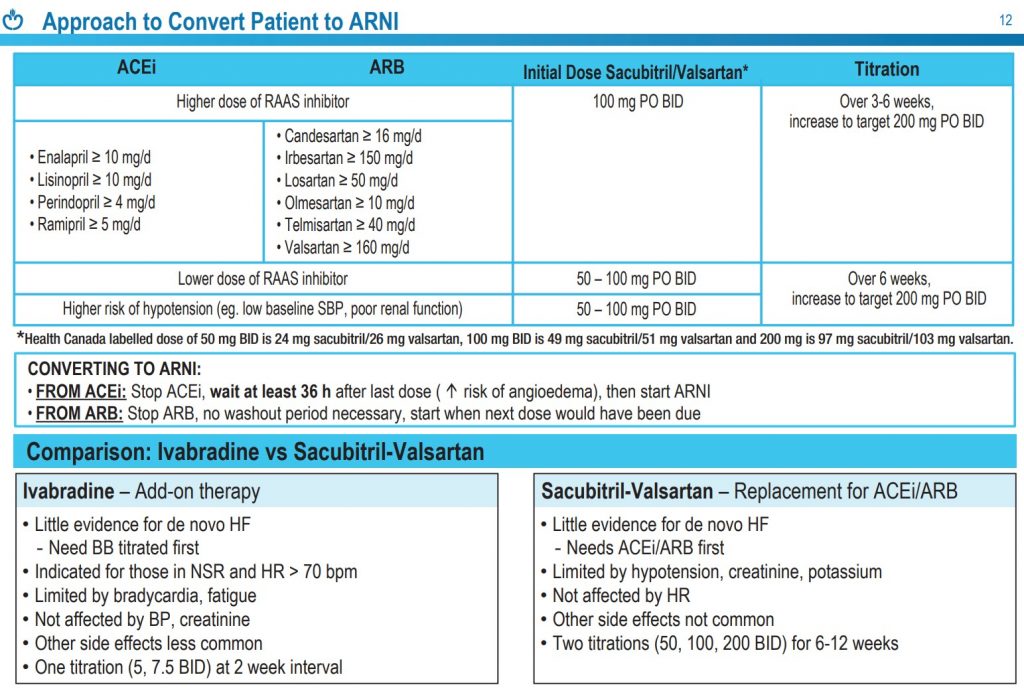
Angiotensin Receptor-Neprilysin Inhibitors (ARNi)
- Recommended to be used in place of ACEi or ARB in patients with HFrEF who are symptomatic despite GDMT to reduce risk of cardiovascular death, HF hospitalizations, and symptoms (PARAGON-HF Trial )
- Notes: ARNi can be directly substituted from ARB without washout period, but when switching from ACEi to ARNi a washout period of at least 36 hours is required. ARNi cannot be used in anyone with a history of angioedema.
Ivabradine
- Recommended in patients with HFrEF who are symptomatic despite GDMT, with a resting heart rate >70, in sinus rhythm, and a previous hospitalization in the last 12 months to reduce risk of cardiovascular death and HF hospitalizations (SHIFT Trial)
- Notes: Beta blockers should be titrated to max dose and Ivabradine added on top. Ivabradine does not affect cardiac contractility or blood pressure. Does not work if patient is in atrial fibrillation.
- SGLT-II Inhibitors
- SGLT-II inhibitors such as dapagliflozin 10mg daily recommended in patients with HFrEF (EF < 40%) with or without diabetes to improve symptoms, quality of life, reduce hospitalizations, and cardiovascular mortality (DAPA-HF Trial)
- Potential adverse effects:
- Contraindicated in Type I DM
- Most common adverse effect are genital mycotic infections (GMI). Women (10-15% risk), previous GMI and uncircumcised men are at highest risk.
- GMI can be managed with antifungal drugs and do not require discontinuation.
- SGLT-II inhibitors might result in temporary reduction in eGFR up to 15%, which generally resolves in 1-3mo.
- Do not cause hypoglycemia
- Should be held in setting of concominant dehydrating illness as part of “Sick Day Plan”
- Associated with diabetic ketoacidosis (0.1% incidence), with normal or modestly elevated blood glucose level. Measurement of serum ketones is required.
Hydralazine and Isosorbide Dinitrate
- In addition to GDMT, recommended in HFrEF in black patients, patients with advanced symptoms and patients unable to tolerate ACEi/ARB/ARNi due to renal dysfunction or hyperkalemia
*See graphic above for target doses of medications
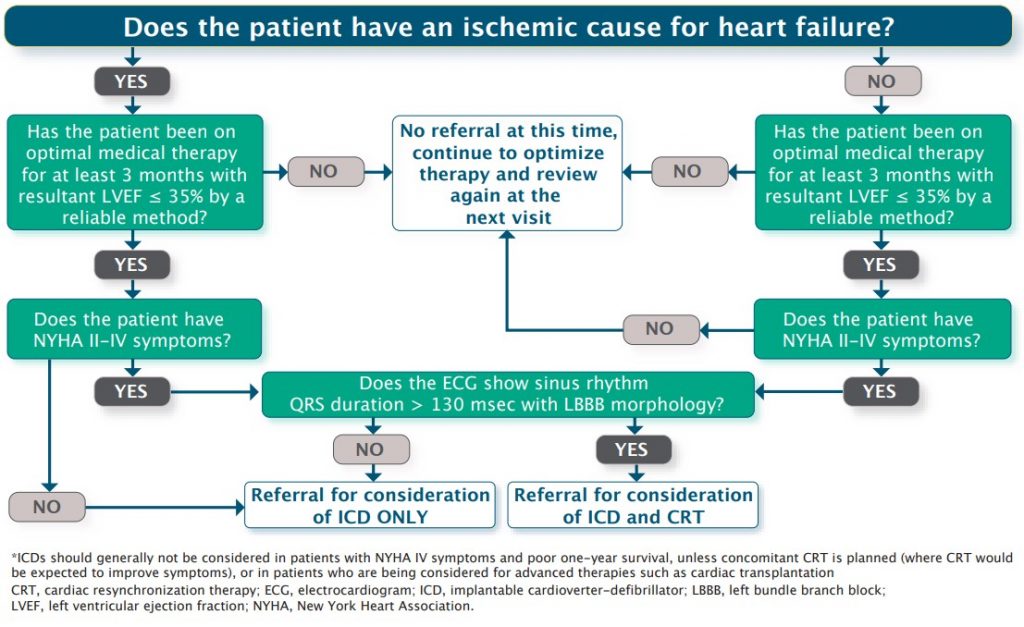
Device Therapy
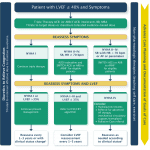
- ICD recommended in patients with HFrEF and hemodynamically significant or sustained ventricular arrhythmia (secondary prevention)
- For secondary prevention ICD indications, please see graphic.
- CRT is recommended in patients in sinus rhythm, NYHA class II-IV despite optimal medical therapy, EF < 35% and LBBB QRS ≥ 130ms (or non LBBB ≥ 150ms)
Advanced Therapy
- Advanced heart failure management strategies such as cardiac transplantation, mechanical support, inotropic support, and palliation will not be discussed in this topic.
- Patients with advanced heart failure who continue to have NYHA III/IV symptoms despite GDMT should have consultation with a specialist with experience in advanced heart failure.
Treatment (HFpEF)
- Recommend treating hypertension as per the Canadian Hypertension Guidelines
- Candesartan and spironolactone can be considered to reduce hospitalizations (weak recommendations)
- Loop diuretics should be used at minimum required doses for symptoms of congestion and peripheral edema
- RCT involving saccubitril/valsartan did not show statistically significant reduction in outcomes.
- RCTs with SGLT-II inhibitors have not shown reductions in hard outcomes. However, patients may qualify for SGLT-II inhibitors for other indications (such as diabetes, kidney disease and cardiovascular disease)
Further Reading
- 2017 CCS: Management of Heart Failure (html) (pdf) (pocketcard)
- 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure (html) (pdf)
- 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure (html)
- 2020 CCS/CHFS: Heart Failure Guidelines (html) (pdf)
Authors
- Authors: Drs. Pavel Antiperovitch (MD, FRCPC, Cardiology Fellow), Atul Jaidka (MD, FRCPC, Cardiology Fellow), and Dr. Omar Gilani (MD, FRCPC, Internal Medicine Resident)
- Staff Reviewer: Dr. Atul Jaidka (MD, FRCPC[Cardiology])
- Copy Editor: Perri Deacon (medical student)
- Last Updated: Jan 23, 2023
- Comments or questions please email feedback@cardioguide.ca