Introduction
- Cardiogenic Shock (CS) is associated with high rates of morbidity and mortality
- Often poses a therapeutic challenge for clinicians
- Caused by severe impairment in myocardial performance with diminished CO, end-organ hypoperfusion, hypoxia
- AMI –> accounts for 81% of cases
- Contemporary studies –> limited by lack of uniformity
- Heterogenous patient populations
- Heterogenous definitions of shock
Cardiogenic Shock Definition - AHA Scientific Statement 2017
- “CS is a low-cardiac-output (CO) state resulting in life-threatening end-organ hypoperfusion and hypoxia”
- Overall, “leads to a state in which ineffective CO caused by primary cardiac disorder results in both clinical and biochemical manifestations of inadequate tissue perfusion”
- Acute cardiac hemodynamic instability may result from disorders that impair function of the myocardium, valves, conduction system, pericardium (either in isolation or in combination)
Epidemiology
- CS complicated 5-10% of AMI
- Leading cause of death in AMI
- STEMI > NSTEMI (>2-fold increased risk)
- Higher risk groups
- Women
- Age >75
- In-hospital mortality has improved (still 35 – 40%)
- 12-month mortality unchanged over 2 decade (approx. 50%)
- Apart from culprit vessel revascularization for AMI, no other intervention has demonstrated an improvement in short-term survival among patients with CS
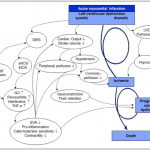
Pathophysiology
- Primary insult = reduced myocardial contractility –> decreased CO
- Inadequate circulatory compensation may also contribute to shock
- Peripheral vasoconstriction
- End-organ damage
- Systemic inflammation –> Patients with “mixed picture” higher risk of mortality
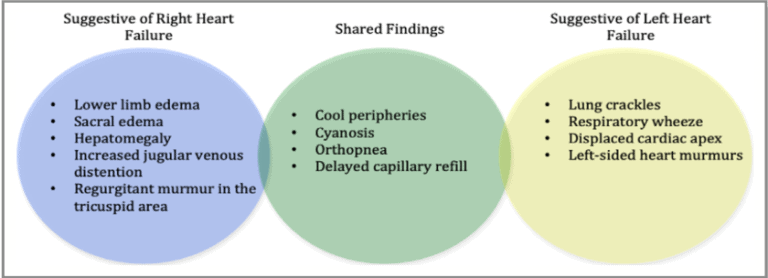
Clinical Presentation and Physical Exam
- Clinically –> persistent hypotension unresponsive to volume replacement and is accompanied by clinical features of endo-organ hypoperfusion requiring intervention with pharmacological or mechanical support
- Classic “cold & wet” phenotype (see below) –> most common; 2/3 of presentations
Differential Diagnosis of Shock
- ***CHAOS***
- Cardiogenic
- Hypovolemic
- Anaphylactic
- Obstructive
- Systemic (neurogenic, distributive)
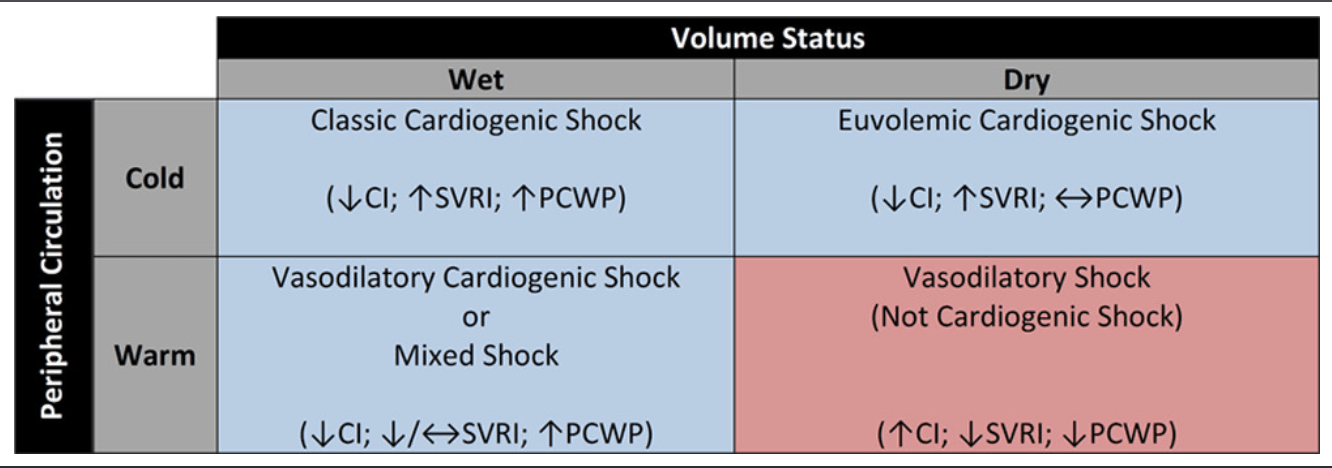
Classification and Risk Stratification
- Multiple classifications exist:
- Two uncommon but hemodynamically distinct entities:
- Normotensive CS
- 2% of the SHOCK trial
- Peripheral hypoperfusion, despite SBP >90
- Comparable CI, PCWP, LVEF vs. other patients, but higher SVR
- Highlights importance of “relative” hypotension***
- Right ventricular CS
- 3% of the SHOCK trial
- Severity of shock may depend of degree of both RV and LV ischemia
- Characterized by –> higher CVP, LVEF; lower PASP
- Similar CI, PCWP
- Classic hemodynamic definition of RV infarction
- CVP / PCWP >/= 0.8
- Normotensive CS
Investigations
- ECG
- Important to assess for ischemia/STEMI
- CXR
- Degree of pulmonary edema
- Echo / POCUS
- Critical to determine etiology of cardiogenic shock (RV, LV, biventricular, valve, etc.)
- Cardiac biomarkers
- Assess of ischemic injury
- BUN/Cr
- Cr > 117 –> higher mortality in IABP-SHOCK II trial
- Liver enzymes/function
- Can suggest hepatic congestion and further evidence of end-organ damage
- Glucose
- Admission hyperglycemia –> higher mortality in IABP-SHOCK II trial
- Lactate
- Arterial lactate –> better established evidence
- Blood gas
- Response to therapy
- Central venous blood gas can offer insight into tissue oxygenation
- Bicarbonate
- Low bicarb –> earlier change vs. lactate in shock; better predictor of 30d mortality vs. peak lactate
- BNP
- Independent prognostic indicator of survival in CS
- Low BNP –> argues against CS when hypotension is present
Stabilization and Resuscitation Strategies
Approach
- Volume Management
- Often very difficult to assess volume status, esp. in AMI
- Some patients may benefit from intravenous volumes esp. RV infarct patients since they are preload dependent. Others benefit from diuresis “cold and wet” or frank pulmonary edema.
- Definitive invasive measurement of filling pressures with RHC recommended for patients with unclear cause of shock or volume status
- Hemodynamic monitoring
- Art line, Cardiac monitor, SpO2, Temperature, Urine output, Mixed venous blood gas (+/- pulmonary artery catheter)
- Oxygenation & ventilation
- If intubation required, low tidal volume (5-7ml/kg) –> decreased incidence of right ventricular failure.
- Positive pressure ventilation may worsen RV failure since it will increase pulmonary vascular resistance (PVR) and worsen pulmonary pressures -> in this case target low PEEP strategy
- Positive Pressure ventilation may help isolated LV dysfunction since will reduce afterload and decrease preload which would be beneficial in patient with high systemic vascular resistance (SVR) and volume overloaded patients
- Hemodynamic goals
- Vary from patient to patient
- No umbrella suggestion
- Consider risks of increased support vs. increased cardiac demand and arrhythmia risk
- Patient-specific titration of support to adequacy of end-organ perfusion
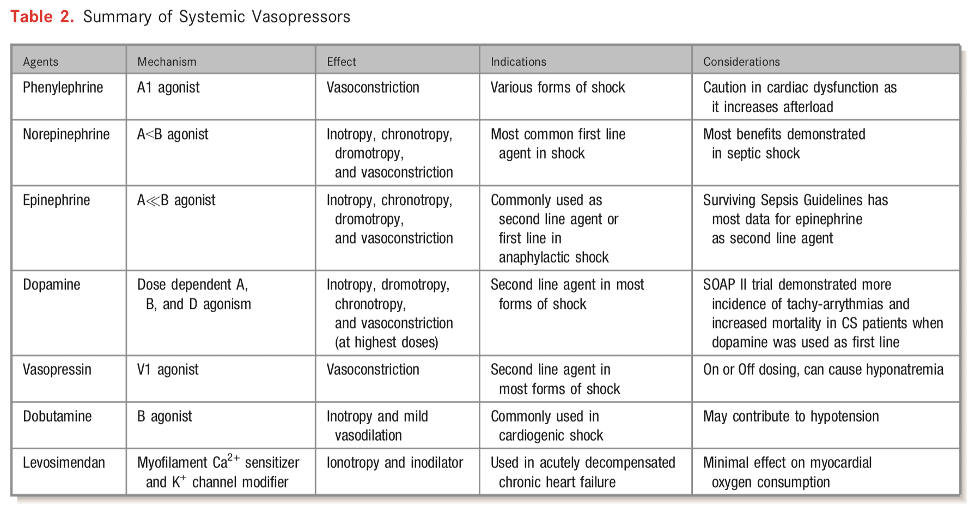
- Vasopressor support
- Very few clinical trials evaluating vasopressors/inotropes in CS
- Norepinephrine generally first line agent
- SOAP II trial — norepinephrine as first line agent in patients with shock was associated with less arrhythmia vs. dopamine [in the CS subgroup]
- There has been a small randomized trial comparing norepinephrine vs epinephrine in cardiogenic shock from MI (Pump Dysfunction) and found that norepinephrine was superior to epinephrine. Epinephrine resulted in more refractory shock cases and worsening metabolics including lactic acidosis but no mortality difference between the groups.
Milrinone vs Dobutamine
Typically, patients are started an ionodilator such as milrinone and dobutamine. There are important considerations when using these medications that may sway a clinician to use one or the other.
- Onset/Half-life:
- Dobutamine has a very quick onset (1-10minutes) and a very short half-life (2 minutes). This has pharmacological advantages for being able to titrate therapy and discontinue therapy should the patient’s hemodynamics dramatically change (i.e. Hypotension).
- Milrinone on the other hand slightly longer onset of action (5-15 minutes) but more importantly has a very long half-life (2.4 hours) this is even longer in patients with renal dysfunction.
- Hypotension/Reduction in SVR:
- Generally, Milrinone causes more hypotension and is more potent at reducing systemic vascular resistance than Dobutamine.
- This may be a desired effect in a cardiogenic shock patient if hypertensive or with profoundly elevated SVR.
- Renal Failure:
- Milrinone is renally cleared and needs to be renally adjusted.
- There is a risk of Milrinone accumulation which can lead to severe hypotension.
- Beta- Blocker Use:
- Milrinone is generally preferred in patients on chronic beta-blockers since their use causes down-regulation of beta-receptors and will make Dobutamine less effective.
- This can sometimes be overcome by a higher dose of Dobutamine.
Hemodynamic Approach
- There is no one way or “cookie-cutter” approach to managing cardiogenic shock.
- Important considerations include Isolated right ventricular dysfunction, Isolated left ventricular dysfunction, biventricular failure, pulmonary hypertension, etiology of shock, arrythmias, valvular disease, these factors drastically effect how cardiogenic shock is managed including therapeutic options that can be provided to patients.
- See table to right/below from AHA that describes tailoring vasoactive management depending on phenotype
- Preferred Pressor: There may be times that a specific pressor is desired. This is generally a non-evidence based approach but often relies on pharmacological principles. For example, a patient with severe or acute pulmonary hypertension with hypotension, Vasopressin may be the preferred agent of choice since it will increase blood pressure but not effect pulmonary vascular resistance.
Renal Failure
- Continuous Renal Replacement Therapy (CRRT)
- AKI occurs in 13-28% of CS
- 20% of patients with AKI will require CRRT
- Consider when
- Cr >/=2 x baseline
- Urine output <0.5ml/kg/hr over >/=12h
- Acid/base disturbances, electrolyte disturbances
- Refractory volume overload
Advanced Management Strategies
Internal Medicine can skip this section
Mechanical support
- Paucity of high-quality evidence to support the routine use of MCS as therapeutic adjunct
- AHA recommendation — “patients with persistent CS, with or without end-organ hypoperfusion, should be evaluated for MCS candidacy by multidisciplinary team with expertise in the selection, implantation, and management of MCS devices”
- MCS for:
- Bridge to recovery
- Bridge to bridge
- Bridge to transplant
- Bridge to decision
- INTERMACS registry reveals decline in use of durable MCS for INTERMACS profile 1 and 2 patients due to high mortality rates despite MCS implantation (38% 30d mortality)
- Consequently, recommendations support use of temporary MCS for INTERMACS profile 1 and 2
- Select temporary MCS options
- IABP — CO 0.5-1L/min
- Most widely used temporary MCS device
- 7-8Fr sheath
- Impella 2.5, Impella CP — 2.5-4L/min
- 11Fr sheath
- Impella 5 — 5L/min
- 22Fr sheath requiring surgical cutdown
- Non-durable VADS
- Tandem Heart
- Centrimag
- VA ECMO
- Used to support both CV system and respiratory system
- AHA statement –> “VA-ECMO should be the preferred temporary MCS option when there is poor oxygenation that is not expected to rapidly improve with an alternative temporary MCS device or during resuscitation”
- Relative contraindications
- Age > 75
- Life expectancy < 1 year
- Severe PVD
- Advanced liver disease
- Contraindications to systemic anticoagulation
- Neurological injury / disability
- Complications
- Distal limb ischemia
- Thromboembolism
- Stroke
- Bleeding
- Hemolysis
- Infection
- AV insufficiency
- Increased LV afterload –> inadequate unloading of LV
- Usually requires –> IABP / Impella, atrial septostomy
- IABP — CO 0.5-1L/min
Durable MCS & transplantation
- Reviewed elsewhere
Reperfusion and Revascularization
- The mainstay evidence-based therapeutic intervention for patients with AMI and CS
- Fibrinolytic therapy
- Very few placebo controlled trials have enrolled patients with CS
- GUSTO-1 trial –> no mortality benefit in any fibrinolytic strategy in CS (approx. 3000 patients)
- Only considered in patients with STEMI + CS in whom invasive approach in timely fashion is not possible
- PCI strategy
- SHOCK trial –> benefit to PCI in CS
- ? Culprit vs. Complete revascularization in CS
- CULPRIT-SHOCK –> benefit for culprit-only PCI compared to complete revasc.
- Discordant results in DANAMI-3, PRAMI, CvLPRIT
- KAMIR-NIH –> benefit for complete revasc. compared to culprit-only
- OVERALL –> discordant results; need for more data
- Evaluate on case-by-case basis
- CULPRIT-SHOCK –> benefit for culprit-only PCI compared to complete revasc.
- Early invasive vs. delayed strategy in CS
- SMASH –> no significant reduction in mortality in early invasive strategy (only 55 patients)
- SHOCK –> no difference in 30d all-cause mortality; however, lower mortality at 6 and 12 months in early invasive arm (302 patients)
- OVERALL –> AHA recommends early invasive strategy for all suitable patients with suspected ACS-associated CS
Further Reading
- Contemporary Management of Cardiogenic Shock: A Scientific Statement From the American Heart Association. Sean Van Diepen et. al. 2017. (html)
- Cardiogenic Shock. American Heart Association. Valdahpour et al. 2019. (html)
- SCAI Clinical Expert Consensus Statement on the Classification of Cardiogenic Shock. Catheterization and Cardiovascular Interventions. David Baren et al. 2019. (html)
- Epinephrine Versus Norepinephrine for Cardiogenic Shock After Acute Myocardial Infarction. Journal of American College of Cardiology. Bruno Levy et al. 2018. (html)
Authors
- Authors: Dr. Daniel Durocher (MD, FRCPC, ICU Fellow)
- Reviewer: Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Staff Reviewer: Pending (MD, FRCPC[Cardiology])
- Last Updated: May 7, 2021
- Comments or questions please email feedback@cardioguide.ca