- For diagnosis, see “Diagnosis of Bradycardia”
Acronyms
ACLS – Acute Cardiovascular Life Support
ASD – Atrial Septal Defect
AV – Atrioventricular
CRT – Cardiac Resynchronization Therapy
EP Study – Electrophysiological Study
ICD – Implantable Cardioverter Defibrillator
LVEF – Left Ventricular Ejection Fraction
MRI – Magenetic Resonance Imaging
PFO – Patent Foramen Ovale
RCA – Right Coronary Artery
RV – Right Ventricle
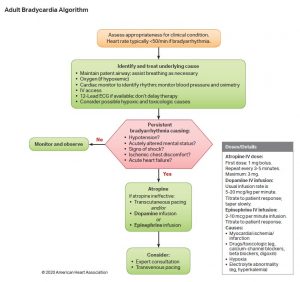
Acute Management
Approach to Management:
Hemodynamically Unstable Patient:
- Follow ACLS Algorithm.
- Administer atropine 1 mg IV q3-5 minutes for a total dose of 3mg.
- Note: atropine increases sinus rate and can worsen infra-Hisian block due to increased activation of diseased tissue.
- Many cardiologists skip atropine administration
- Consider administrating ONE of the following chronotropic agents if the patient remains symptomatic despite atropine, and temporary pacing is not available or is unsuccessful.
- Epinephrine 2-10 mcg/min IV infusion titrate to effect.
- Usual dose is 0.1-0.5 mcg/kg/min.
- Dopamine 5-20mcg/kg/min IV infusion, can titrate to a maximum of 50mcg/kg/min for response (note that doses >20mcg/kg/min may increase the risk of tachyarrhythmias).
- Isoproterenol 2-10mcg/min continuous IV infusion, titrate to response.
- Epinephrine 2-10 mcg/min IV infusion titrate to effect.
- Initiate temporary cardiac pacing: (see below for indication for temporary pacing)
- Transcutaneous OR
- Transvenous
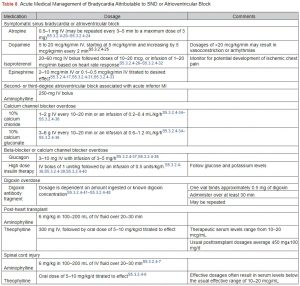
If drug toxicity is suspected, use the appropriate antidote. See table.
Transvenous / Transcutaneous Pacing
- Indications:
- Medically refractory symptomatic or hemodynamically unstable bradycardia (includes markers of cardiogenic shock such as reduced urine output or altered mental state).
- Bradycardia associated with a long QT (i.e. QTc > 500ms).
- Unreliable escape rhythm:
- Junctional escape: more stable, usually faster escape rates (>40 BPM). Identified by narrow QRS or QRS identical to prior sinus rhythm. Can defer temporary transvenous pacemaker if no other indication.
- Ventricular escape: less reliable, Wide QRS, usually slower than 40bpm. Almost always require a temporary transvenous pacemaker.
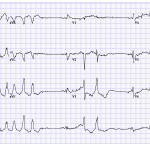
- NOTE: Many patients with AV block or other bradycardias experience syncope or a cardiac arrest not from bradycardia itself, but secondary to the resultant long QT, which can lead to Torsades de pointes (see ECG).
- Transcutaneous pacing
- Temporizing measure – energy is delivered through pads applied to the chest.
- If the patient is conscious, they MUST be sedated because transcutaneous pacing can be very uncomfortable (i.e. midazolam and fentanyl).
- Mechanical capture must be confirmed by palpating a central pulse. Contraction of the chest wall muscles does not suggest capture of myocardium.
- Transvenous pacing
- A central line with an electrical lead passed into the RV cavity.
- Two types exist:
- Soft Balloon-Tipped Wire – has an inflatable balloon, which can be floated with the bloodflow into the RV.
- Fluroscopy/X-Ray is not required.
- Patients with tricuspid regurgitation may be particularly challenging.
- Hard Wire – Need intra-procedural fluoroscopy/X-Ray because the wire is stiff.
- Hard wires are more stable, but carry a higher risk of perforation.
- Soft Balloon-Tipped Wire – has an inflatable balloon, which can be floated with the bloodflow into the RV.
Pacing Indications
- The mainstay of treating bradycardia is pacemaker implantation.
- Any symptomatic bradycardia requires pacing. Some bradycardias have a good prognosis (AV nodal), and risks/benefits of pacemaker for symptomatic relief need to be discussed.
- However, certain conditions carry a poor prognosis, marked by progressive conduction system disease. For those conditions, symptoms are not required, and pacing is indicated prophylactically:
- Infra-His block (i.e. Mobitz II, most complete AV block etc..), and alternating bundle branch blocks.
- Conditions must be irreversible.
- Can consider EP study or empiric pacing for syncope + bundle branch block.
| Summarized from AHA 2019 Pacing Guidelines |
| Indications for pacing |
|---|
***MUST BE IRREVERSIBLE |
Myocardial Infarction and AV block
- Class I Indications:
- In patients presenting with an acute MI with Mobitz type II second-degree AV block, high-grade AV block, alternating bundle-branch block, or third-degree AV block (persistent or infranodal), permanent pacing is indicated after a waiting period.
- NO pacing required (Class III) for:
- Acute MI and transient AV block that resolves.
- Acute MI with new BBB or isolated fascicular block in absence of second or third-degree AV block.
- Patients with inferior (RCA) STEMI commonly present with AV block.
- The most common mechanism is Bezold–Jarisch reflex, which is a neurologically (vagal) mediated AV block at the level of the AV node.
- This is usually temporary and does not require pacing.
- Atropine can be used for temporary control if the patient is symptomatic.
- Chronotropic drugs need to be avoided because they can increase myocardial demand, which may increase infarct size.
- Temporary transvenous pacing wires are avoided due to the theoretical risk of perforating an ischemic RV. However, transvenous pacing may be required if the patient has hemodynamically unstable bradycardia.
- An acute STEMI can cause AV nodal ischemia and result in AV block. This usually resolves, and is very uncommon due to dual blood supply to the AV node.
- The most common mechanism is Bezold–Jarisch reflex, which is a neurologically (vagal) mediated AV block at the level of the AV node.
Pre-Pacemaker Workup
- History/physical to rule out active infection and reversible causes.
- Echocardiogram to assess LVEF if the patient is a candidate for ICD/CRT, and rule out ASD/PFO.
- Laboratory investigations to rule out reversible metabolic causes.
- ** Young patients with AV block must be carefully evaluated for secondary conditions, such as connective tissue diseases, autoimmune diseases, and sarcoidosis.
- Sarcoidosis with cardiac involvement is an important cause of AV block. A screening chest X-ray is reasonable and possibly a CT chest to assess for mediastinal lymphadenopathy. Sarcoidosis can be confirmed with a cardiac MRI/PET and/or biopsy.
- It is preferable to obtain a cardiac MRI prior to device implantation, as metal artifact can make interpretation challenging.
- Authors: Drs. Yehia Fanous (MD, FRCPC, Internal Medicine Resident), Atul Jaidka (MD, FRCPC, Cardiology Fellow), Dr. Pavel Antiperovitch (MD, FRCPC[Cardiology])
- Staff Reviewer: Dr. Pavel Antiperovitch (MD, FRCPC[Cardiology])
- Copy Editor: Donald Bastin
- Last Updated: Nov 13, 2021
- Comments or questions please email feedback@cardioguide.ca