Diagnosis
- Definition:
- Atrial rhythm ≥ 100bpm initiated from a discrete origin
- Ventricular rate varies depending on AV nodal conduction
- Can be paroxysmal, sustained, or incessant
- ECG Features
- The key is to find the P-waves!
- Depending on velocity of AV conduction, P-waves can be located anywhere in the cycle (commonly in the QRS or T-wave)
- P-waves often have different morphology to sinus P-waves (compare to sinus ECG)
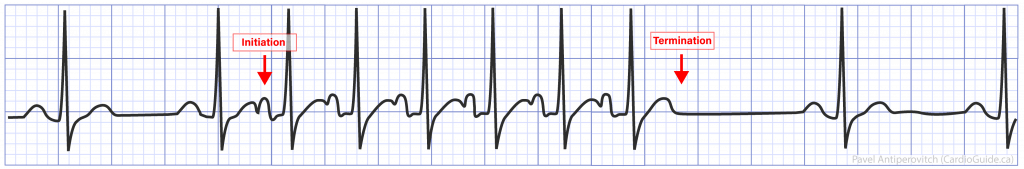
-
- Caveat: P-wave morphology can match sinus P-waves when the focus is close to the sinus node.
- P-wave morphology can resemble retro-conducted P-waves if the origin is low in the atrium or close to the AV node.
-
- Sometimes a “Warm-Up” and “Cool-Off” phenomenon can be seen where the tachycardia accelerates and gradually slows down before terminating.
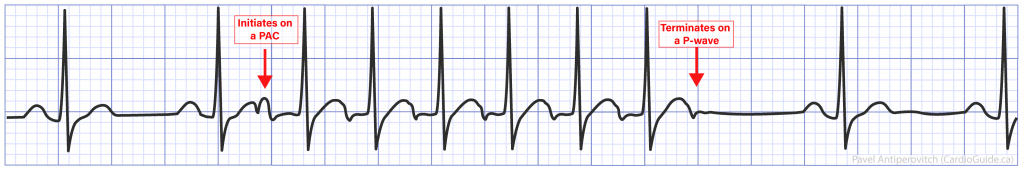
- SVT that terminates on a P-wave is significantly less likely to be AT
- Explanation: If a tachycardia terminates on a P-wave, the atrial focus must stop firing, and the AV node must block on the same beat. Both of these events are statistically unlikely to happen on the same beat.
- The key is to find the P-waves!
Response To Adenosine
- Adenosine blocks the AV node, which stops ventricular activation, revealing AT P-waves.
- Compare these P-waves to the sinus ECG.
- Usually P-waves are discrete and separated by an isoeletric period
- Tachycardia continues after adenosine effect wears off.
- NOTE: Some atrial tachycardias are adenosine-sensitive, and can slow down or terminate with adenosine.
Localizing Atrial Origin (Advanced)
- Negative P wave in lead I and aVL suggests LA origin
- V1 is negative –> lateral RA
- V1 is biphasic or positive –> Septal RA and LA
- Negative in inferior leads –> Inferior origin
- Positive in inferior leads –> Superior origin
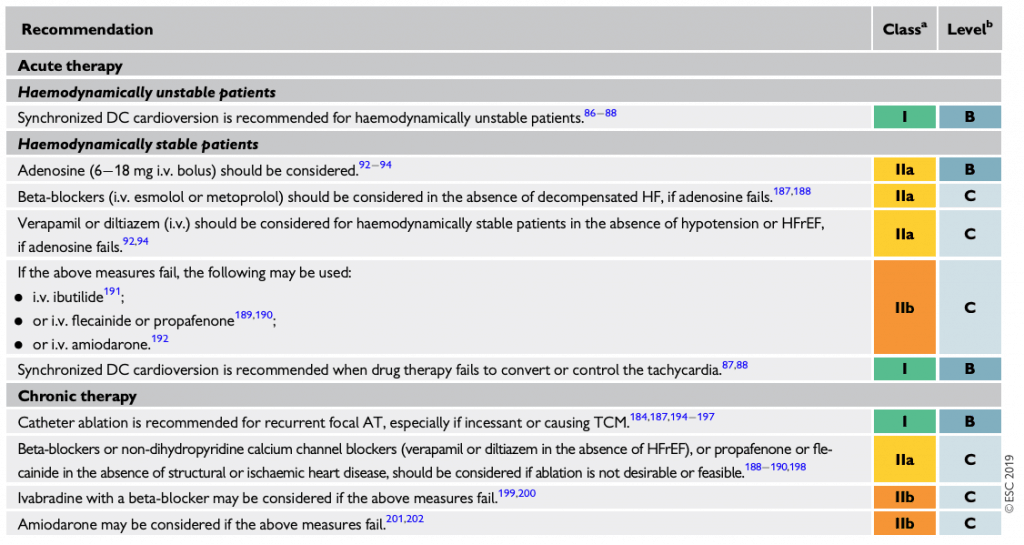
Acute Therapy
If unstable –> Cardioversion (Class IA)
- Identify and treat associated conditions:
- LA stretch (HF, CMP, HTN), MI, PE, infection, alcohol, electrolytes, cocaine/stimulants, theophyline
- Adenosine (IIA)
- Rarely work.
- Adenosine can convert DAD-triggered AT
- B-Blockers (IIA)
- Can terminate or slow the rate
- Avoid in decompensated HF
- Metoprolol 2.5-5mg IV over 2-5min (max 15mg)
- CCB (IIA)
- Avoid in Hypotension and HFrEF
- Diltiazem 20mg IV bolus over 2min, repeat q15min
- Verapamil: 5-10mg IV over 2min. Additional 10mg IV can be given after 15-30min
4. Class IA, IC, and III drugs can prolong refractoriness or suppress automaticity
-
- IV Ibutilide
- IV flecainide or propafenone
- IV Amiodarone (preferred if acute HF or hypotensive
5. Cardioversion may not be effective due to automaticity (especially incessant AT). If it works, tachycardia can reinitiate.
6. IV Amiodarone
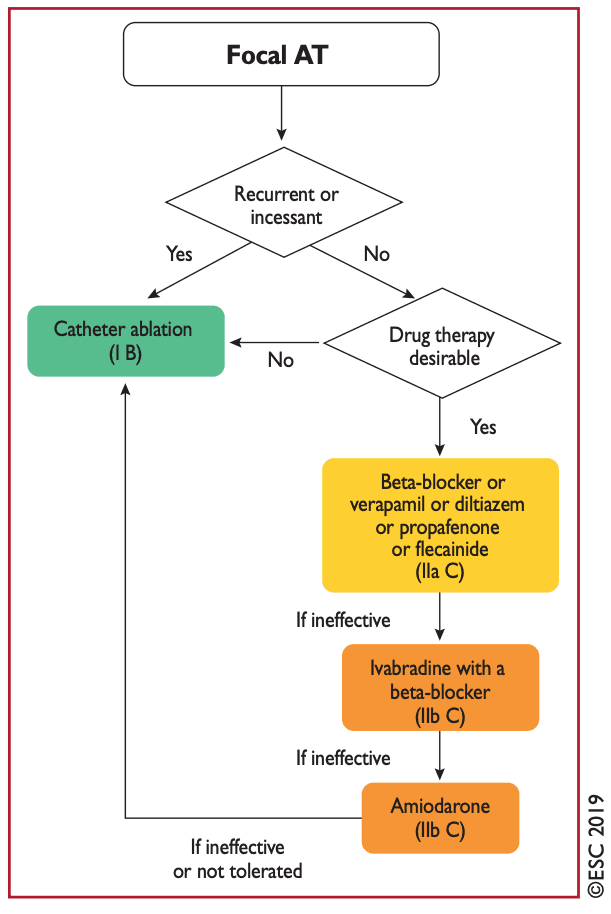
Chronic Therapy
- If rare and brief episodes, may not need chronic therapy
- Anticoagulation not necessary (low risk of embolism)
- 1st line: Catheter Ablation is Preferred (Class I)
- Especially if insessant or TCM
- Ablation is effective (75-100% success rate)
- Medication (if ablation not feasible/desirable)
- 2nd line: CCB and BB may be effective (IIA)
- If one fails, try another
- 2nd line: Class IC may be effective
- Flecainide and propafenone (if no structural/ischemic heart disease) (IIA)
- (Decide with experts)
- Ivabradine can be effective for focal AT (give with BB)
- 3rd line: Amiodarone (avoid due to side-effect profile)
- 2nd line: CCB and BB may be effective (IIA)
- If all options fail –> AV Node Ablation with pacing