Introduction
Stenosis of the descending aorta
(in the area of ligamentum arteriosum)
- Rare in desc or abdominal aorta
- Usually discrete (sometimes aortic hypoplasia)
- Majority distal to L-subclavian
- Pathophysiology (proposed)
- Cells in the PDA migrate to the aorta.
- After birth, cells exposed to high pO2 (sVO2 is 70% in utero), causing cytokine activation
- Results in narrowing/closure of the PDA and aorta
- Associated with Turner’s Syndrome
(+Bicuspid Aortic Valve) - “Aortopathy”
- Intima abnormal in entire aorta, and it is
- Susceptible to dissection/dilation (not just coarct site)
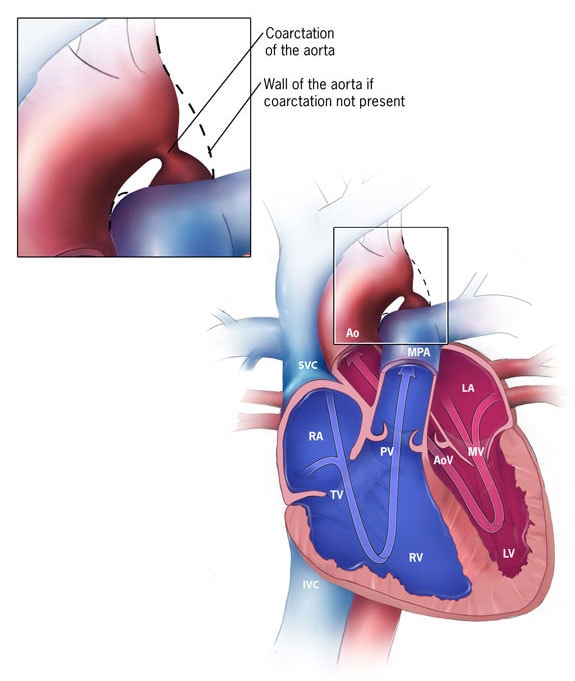
Classification
- Types (Pediatrics)
- Pre-Ductal (worse, relies on PDA, once PDA closes, circulation is compromised)
- Juxta-Ductal
- Post-Ductal (better b/c develops collaterals in-utero)
- Types:
- Simple: No other cardiac lesions (50%)
- Complex: associated with other lesions (50%)
Associations
- Bicuspid Aortic Valve (80%) = worse outcomes! (aortic syndromes)
- Berry (intracranial) aneurysms of the circle of Willis (3-5%)
- Brachiocephalic anomalies (5%)
- I.e. anomalous origin of R-subclavian
- Collaterals
- Anterior –> IMA
- Posterior –> Intercostal Arteries
- VSD
Presentation / History
- Symptoms: (often absent)
- Headaches
- Exertional Leg Fatigue
- Vitals
- Upper limb hypertension
- Differential arm-leg pulses
- Incidental Murmur
- Severe Presentation:
- Heart Failure (30-40yo) (28%)
- Aortic rupture/dissection (21%)
- Cerebral Hemorrhage (12%)
- Premature CAD
- Aortic Valve Disease
Diagnosis
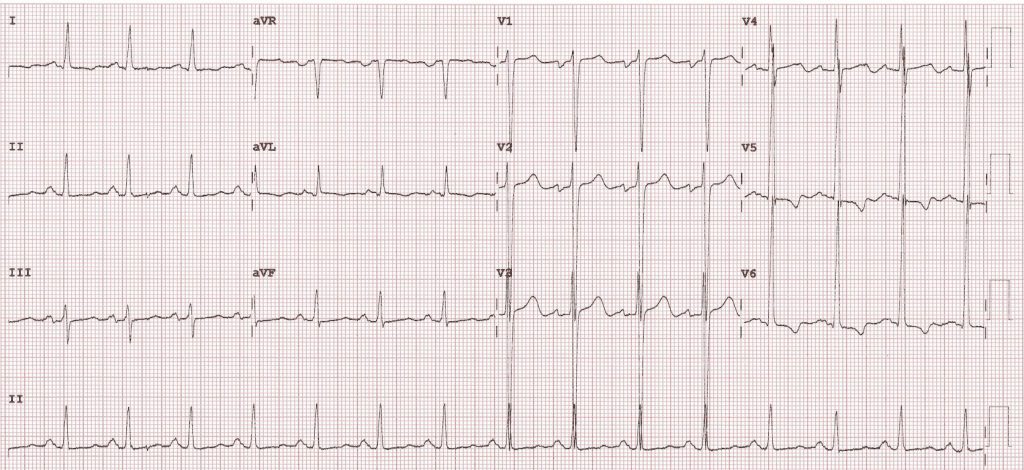
Physical Exam
- Blood Pressure –> Upper & Lower Limb (>20 sBP differential)
- Cardiac
- Systolic murmur LSE–> continuous
- Collaterals cause murmurs radiate to back
- 4th sound w/ LVH & HTN
- Loud A2 if hypertension
- Ejection click (bicuspid AoV)
- Delayed femoral pulses
- Radio-femoral delay
Chest Xray
Management
- Workup:
- ECG, Chest Xray, Echo
- MRI is very important (aneurysms/collaterals etc..)
- CTA/MRA of head! (berry aneurysms)
- Cath –> gradient (can treat percutaneously)
Significant Aortic Coarctation - Peak pull back gradient of > 20 mmhg across coarctation site on angiography
OR - Peak pullback > 10 mmHg and collaterals
(Canadian guidelines don’t define cutoff if collaterals present)
- Peak pull back gradient of > 20 mmhg across coarctation site on angiography
Indications for repair
- Surgical vs. percutaneous
- (Generally percutaneous is preferred unless additional problems coexist)
- Surgical Techniques:
- End-to-end anastomosis (preferred)
- Subclavian flap aortoplasty (children – supply to arm may be compromized)
- Dacron patch
- Tube graft
| AHA 2018 Guidelines |
| Indications for Repair (AHA 2018) |
|---|
|
| Indications for Repair (Canadian 2008) |
|---|
| CachNet Guidelines 2018 (Canada) |
|
Ongoing Care (Post-Op)
- Surgery is NOT a cure
- Remember: Aortopathy!
- 80% have HTN (AHA 2018) at 30y
- Surgival is LOWER than population (30y survival 72%)
- Age of repair predicts survival (< 20yo survival better but not normal)
- Need lifelong cardiology follow-up
- Premature death due to:
- Coronary Artery Disease
- Heart Failure
- Stroke
- Post-Repair Complications:
- Re-Coarctation
- Dacron patch aneurysms
- Aortic emergencies (dissection/aneurysm/rupture)
- New HTN must be treated aggressively with GDMT
- Exclude re-coarctation
- B-blockers often quoted first line
- Screen for HTN with exercise/rest/ambulatory (AHA 2018)
- MRI Head q5-10 years (Class IIB)
- (10% have aneurysms – AHA 2018)
- Cannot MRI if has a aortic stent
- Follow-up aortic imaging CTA/MRA post-repair (some say q5-10y) (Class I)
- Ambulatory 24-hr BP monitor can be useful (Class IIA)
- Exercise BP testing if patient exercises (Class IIB)