Key Points
- Beta Blockers should be given to post ACS patients with HF or LVEF<40 and considered in all patients
- ACE Inhibitors should be given to post ACS patients with HF, LVEF<40, diabetes, or anterior infarct and considered in all patients.
- MRAs should be given to post ACS patients with LVEF<40 and HF or diabetes (given no renal failure or hyperkalemia)
Cases
Landmark Trials
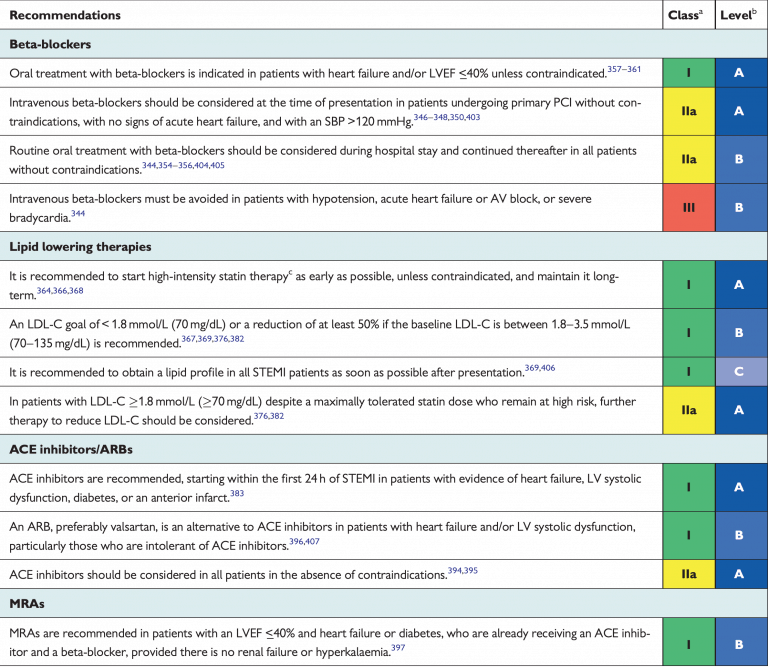
ESC 2017 STEMI Guidelines
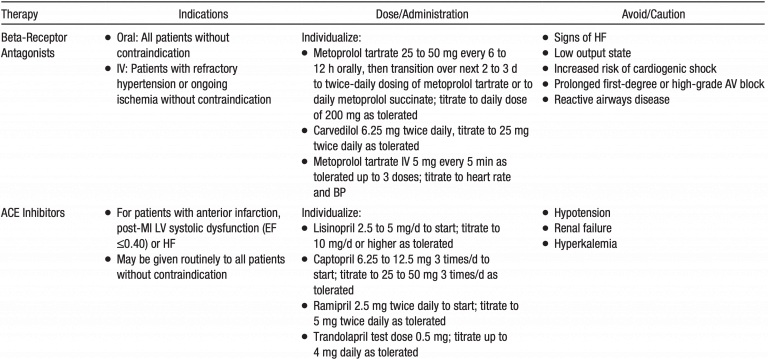
AHA 2013 STEMI Guidelines
MRA: “An aldosterone antagonist should be given to patients with STEMI and no contraindications who are already receiving an ACE inhibitor and beta blocker and who have an EF less than or equal to 0.40 and either symptomatic HF or diabetes mellitus.”
AHA 2014 NSTEMI Guidelines
| Beta Blocker | Class 1 | Oral beta-blocker therapy should be initiated within the first 24 hours in patients who do not have any of the following: 1) signs of HF, 2) evidence of low-output state, 3) increased risk for cardiogenic shock, or 4) other contraindications to beta blockade (eg, PR interval >0.24 second, second- or thirddegree heart block without a cardiac pacemaker, active asthma, or reactive airway disease). (Level of Evidence: A) |
| In patients with concomitant NSTE-ACS, stabilized HF, and reduced systolic function, it is recommended to continue beta-blocker therapy with 1 of the 3 drugs proven to reduce mortality in patients with HF: sustained-release metoprolol succinate, carvedilol, or bisoprolol. (Level of Evidence: C) | ||
| Patients with documented contraindications to beta blockers in the first 24 hours of NSTE-ACS should be re-evaluated to determine their subsequent eligibility. (Level of Evidence: C) | ||
| Class 2a | It is reasonable to continue beta-blocker therapy in patients with normal LV function with NSTEACS. (Level of Evidence: C) | |
| Class 3 (harm) | Administration of intravenous beta blockers is potentially harmful in patients with NSTE-ACS who have risk factors for shock. (Level of Evidence: B) | |
| ACE Inhibitors | Class 1 | ACE inhibitors should be started and continued indefinitely in all patients with LVEF less than 0.40 and in those with hypertension, diabetes mellitus, or stable CKD unless contraindicated. (Level of Evidence: A) |
| ARBs are recommended in patients with HF or MI with LVEF less than 0.40 who are ACE inhibitor intolerant. (Level of Evidence: A) | ||
| Class 2a | ARBs are reasonable in other patients with cardiac or other vascular disease who are ACE inhibitor intolerant. (Level of Evidence: B) | |
| Class 2b | ACE inhibitors may be reasonable in all other patients with cardiac or other vascular disease. (Level of Evidence: B) | |
| MRA | Class 1 | Aldosterone blockade is recommended in patients post–MI without significant renal dysfunction (creatinine >2.5 mg/dL in men or >2.0 mg/dL in women) or hyperkalemia (K+ >5.0 mEq/L) who are receiving therapeutic doses of ACE inhibitor and beta blocker and have a LVEF 0.40 or less, diabetes mellitus, or HF. (Level of Evidence: A) |
Notes: No large RCT studying beta blockers and NSTEMI
Specific Situations
- METOCARD-CINIC: “In patients with anterior Killip class ≤II STEMI undergoing pPCI, early IV metoprolol before reperfusion resulted in higher long-term LVEF, reduced incidence of severe LV systolic dysfunction and ICD indications, and fewer heart failure admissions.”
- EARLY-BAMI: “In a nonrestricted STEMI population, early intravenous metoprolol before PPCI was not associated with a reduction in infarct size. Metoprolol reduced the incidence of malignant arrhythmias in the acute phase and was not associated with an increase in adverse events.”
- ESC Guidelines: “Based on the current available evidence, early administration of i.v. beta-blockers at the time of presentation followed by oral beta-blockers should be considered in haemodynamically stable patients undergoing primary PCI.”
- Yang et al. 2014 (JACC Cardiovascular Interventions): “Beta-blocker therapy at discharge was associated with improved survival in STEMI patients treated with primary PCI.”
- Dondo et al. 2017 (JACC): “Among survivors of hospitalization with AMI who did not have HF or LVSD as recorded in the hospital, the use of β-blockers was not associated with a lower risk of death at any time point up to 1 year.”
- ESC Guidelines: “Based on the current evidence, routine administration of beta-blockers in all post-STEMI patients should be considered”
- AHA Guidelines: All patients without contraindications
- ESC Guidelines: “Acute heart failure, haemodynamic instability, or higher degree AV block”
- AHA Guidelines: “Signs of HF, evidence of a low output state, increased risk for cardiogenic shock,‖ or other contraindications to use of oral beta blockers (PR interval more than 0.24 seconds, second- or third-degree heart block, active asthma, or reactive airways disease)”
- HOPE: “Ramipril significantly reduces the rates of death, myocardial infarction, and stroke in a broad range of high-risk patients who are not known to have a low ejection fraction or heart failure.”
- Includion: History of CAD, CVA, PAD or DM plus one other CV risk factor (HTN, HL, smoking, microalbuminuria)
- EUROPA: “Among patients with stable coronary heart disease without apparent heart failure, perindopril can significantly improve outcome. About 50 patients need to be treated for a period of 4 years to prevent one major cardiovascular event.”
- Coronary artery disease, as documented by: Prior MI (>3 months prior to enrollment), revascularization (>6 months prior to enrollment) or Coronary artery stenosis (≥70%) on angiography
- ESC Guidelines: Treatment with ACE inhibitors is recommended in patients with systolic LV dysfunction or heart failure, hypertension, or diabetes, and should be considered in all STEMI patients.
- REMINDER: “The addition of eplerenone during the acute phase of STEMI was safe and well tolerated. It reduced the primary endpoint over a mean 13 months follow-up mostly because of significantly lower BNP/NT-proBNP levels. Additional studies are needed to clarify the role of early use of MRAs in STEMI patients without heart failure.”
- ALBATROSS: “The study failed to show the benefit of early MRA use in addition to standard therapy in patients admitted for MI.”
- ESC Guidelines: “Future studies will clarify the role of MRA treatment in this setting.”
Beta Blockers:
- ESC: As no study has properly addressed beta-blocker duration to date, no recommendation in this respect can be made.
- AHA: The long-term duration of routine beta-blocker therapy after uncomplicated MI in patients without HF or hypertension has not been prospectively addressed. AHA/ACCF secondary prevention guidelines recommend a 3-year treatment course in this patient subset.
- Further study is needed in this area but in patients without heart failure or hypertension, reasonable to have a discussion with patients and have an informed discussion on the benefits vs risks of indefinite beta blocker therapy.
- Circulation Commentary 2018: “Stopping β-Blockers After Myocardial Infarction – Not so Fast”
ACE Inhibitor:
- Guidelines don’t address duration.
- Given evidence of benefit in stable CAD patients, likely continue for life, especially if hypertension, diabetes, or reduced EF.
MRA:
- Guidelines don’t address duration.
- Given narrow recommendation of reduced EF and data with benefit in this population in the none post ACS setting, likely continue for life.
Improved EF:
- EF improves, whether heart failure medications can be withdrawn is not yet known.
- Lancet Commentary on TRED-HF Study 2018: “Stopping medication for heart failure with improved ejection fraction”
Further Reading
- 2017 ESC: Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation (html) (pdf)
- 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes (html) (pdf)
- 2013 AHA: Guideline for the Management of ST-Elevation Myocardial Infarction (html) (pdf)